J Korean Med Sci.
2009 Aug;24(4):722-728. 10.3346/jkms.2009.24.4.722.
Clinical Features and Prognosis of HLA-B27 Positive and Negative Anterior Uveitis in a Korean Population
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. diham@skku.edu
- KMID: 1779210
- DOI: http://doi.org/10.3346/jkms.2009.24.4.722
Abstract
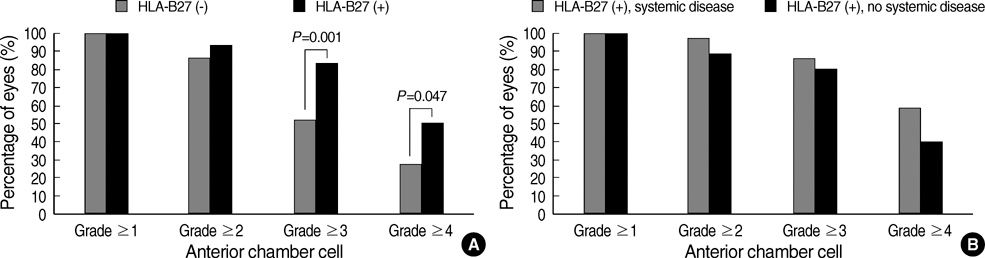
- Clinical features and prognosis of HLA-B27 positive anterior uveitis (AU) were assessed compared with HLA-B27 negative AU in a Korean population, based on the medical records of AU patients seen at a university hospital. Twenty-seven HLA-B27 negative, idiopathic AU patients (group I) and 55 HLA-B27 positive AU patients (group II) were studied. HLA-B27 positive group was further divided into 29 with associated systemic disease (seronegative spondyloarthropathy) (group IIA) and 26 without associated systemic disease (group IIB). Significantly more severe anterior chamber inflammation in terms of anterior chamber cells (P=0.006) and hypopyon formation (P=0.034) was observed with higher frequency of AU attacks (P=0.007) in the HLA-B27 positive group than in the HLA-B27 negative group. Systemic/periocular steroids were required in significantly more patients in the HLA-B27 positive group than in the HLA-B27 negative group (P=0.015). However, no significant differences were observed for final ocular and visual outcomes between these two groups. Associated systemic disease made no significant difference in the clinical features and prognosis in the HLA-B27 positive AU patients. In conclusion, despite more severe inflammation and a higher recurrence rate, HLA-B27 positive AU shows similar good final ocular and visual outcomes compared to HLA-B27 negative, idiopathic AU in a Korean population.
MeSH Terms
-
Adolescent
Adult
Aged
Alleles
Anti-Inflammatory Agents, Non-Steroidal/therapeutic use
Asian Continental Ancestry Group
Case-Control Studies
Female
HLA-B27 Antigen/genetics/*metabolism
Humans
Immunosuppressive Agents/therapeutic use
Korea
Male
Middle Aged
Prognosis
Retrospective Studies
Severity of Illness Index
Steroids/therapeutic use
Uveitis, Anterior/*diagnosis/drug therapy/metabolism
Visual Acuity
Figure
Reference
-
1. Chang JH, Wakefield D. Uveitis: a global perspective. Ocul Immunol Inflamm. 2002. 10:263–279.
Article2. Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol. 2005. 50:364–388.
Article3. Choi DG, Chung H. Clinical analysis of uveitis in Korea. J Korean Ophthalmol Soc. 1989. 30:543–562.4. Oh JW, Kim MH, Yoo JS, Huh W. Analysis of HLA typing in patients with uveitis in Korean population. J Korean Ophthalmol Soc. 1999. 40:104–109.5. Kim MJ, Han YB. Clinical features of HLA-B27 positive and negative acute anterior uveitis. J Korean Ophthalmol Soc. 1999. 40:3065–3070.6. Nussenblatt RB, Whitcup SM. Uveitis: fundamentals and clinical practice. 2004. 3rd ed. Philadelphia: Mosby;275–276.7. Rothova A, Kijlstra A, Buitenhuis HJ. Saari KM, editor. HLA-B27 associated uveitis. A distinct clinical entity? Uveitis Update. 1984. Amsterdam: Elsevier Science Publishers;91–95.8. Wakefield D, Easter J, Penny R. Clinical features of HLA-B27 anterior uveitis. Clin Experiment Ophthalmol. 1984. 12:191–196.
Article9. Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology. 1998. 105:1646–1651.
Article10. Linssen A. B27+ disease versus B27- disease. Scand J Rheumatol Suppl. 1990. 87:111–118.
Article11. Linssen A, Meenken C. Outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis. Am J Ophthalmol. 1995. 120:351–361.
Article12. Rothova A, van Veenedaal WG, Linssen A, Glasius E, Kijlstra A, de Jong PT. Clinical features of acute anterior uveitis. Am J Ophthalmol. 1987. 103:137–145.
Article13. Pathanapitoon K, Suksomboon S, Kunavisarut P, Ausayakhun S, Wattananikorn S, Leetrakool N, Rothova A. HLA-B27-associated acute anterior uveitis in the University Referral Centre in North Thailand: clinical presentation and visual prognosis. Br J Ophthalmol. 2006. 90:1448–1450.
Article14. Tuncer S, Adam YS, Urgancioglu M, Tugal-Tutkun I. Clinical features and outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis in a Turkish patient population. Ocul Immunol Inflamm. 2005. 13:367–373.
Article15. The Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005. 140:509–516.16. Rodriguez A, Akova YA, Pedroza-Seres M, Foster CS. Posterior segment ocular manifestations in patients with HLA-B27-associated uveitis. Ophthalmology. 1994. 101:1267–1274.
Article17. Monnet D, Breban M, Hudry C, Dougados M, Brézin AP. Ophthalmic findings and frequency of extraocular manifestations in patients with HLA-B27 uveitis: a study of 175 cases. Ophthalmology. 2004. 111:802–809.18. Chung YM, Yeh TS, Liu JH. Clinical manifestations of HLA-B27-positive acute anterior uveitis in Chinese. Zhonghua Yi Xue Za Zhi (Taipei). 1989. 43:97–104.19. Lee DY, Shin JC, Choe JK, Park YS. Clinical studies on the relation of HLA B-27 and uveitis. J Korean Ophthalmol Soc. 1997. 38:2141–2146.20. Kim TG, Kim MH, Yoo JS, Huh W. Clinical studies in patients with HLA-B27 positive uveitis. J Korean Ophthalmol Soc. 2000. 41:67–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features of HLA-B27 Positive and Negative Acute Anterior Uveitis
- Analysis of Typing in Patients with Uveitis in Korean Population
- A Case of Acute Anterior Uveitis Associated with HLA-B27 Positivity after Intravitreal Injection of Bevacizumab
- Clinical Studies in Patients with HLA-B 27 Positive Uveitis
- HLA-B27 Positive and HLA-B27 Negative Ankylosing Spondylitis: A Comparative Study in Diagnostic Process and Clinical Features