J Korean Med Sci.
2011 Apr;26(4):583-586. 10.3346/jkms.2011.26.4.583.
Xanthogranulomatous Pancreatitis Presents as a Solid Tumor Mass: A Case Report
- Affiliations
-
- 1Department of Pathology, Inje University Ilsan Paik Hospital, Goyang, Korea. hskim@paik.ac.kr
- 2Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 3Department of Radiology, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 4Department of General Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea.
- KMID: 1777893
- DOI: http://doi.org/10.3346/jkms.2011.26.4.583
Abstract
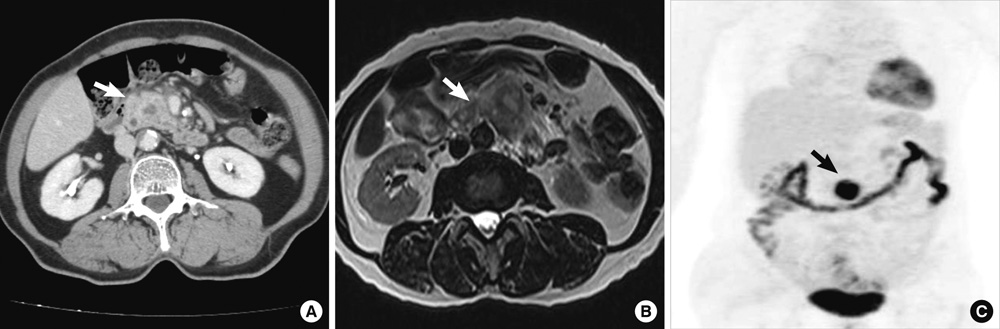
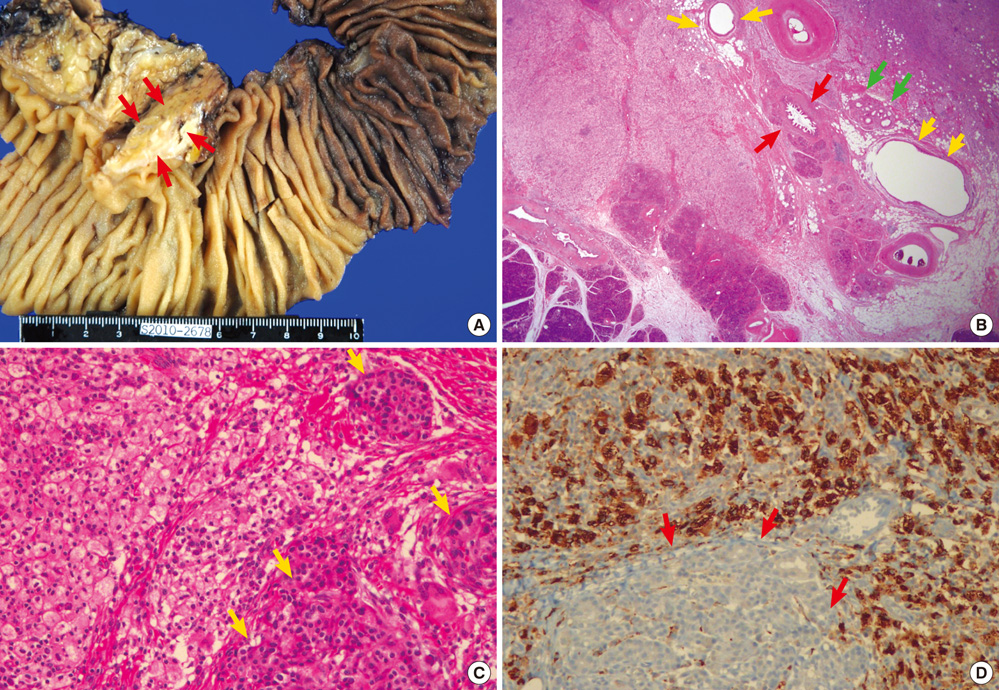
- Xanthogranulomatous inflammation (XGI) is a rare, idiopathic process in which lipid-laden histiocytes are deposited at various locations in the body. Although XGI has been reported to occur in various organs such as the gallbladder, kidney, bone, stomach, colon, appendix, lymph nodes, urachus, and urinary bladder and in soft tissues, xanthogranulomatous pancreatitis (XGP) is extremely rare. Herein, we report a case of XGP occurring in a 70-yr-old woman, who presented with abdominal pain for several months. On physical examination, mild epigastric tenderness was noted. Abdomen CT scan revealed a low attenuated mass in uncinate process of pancreas, suggesting malignant lesion. Whipple's operation was performed and the final pathologic diagnosis was XGP. The patient's post-operative course was uneventful, and no recurrence was found within 7 months of the operation. When a pancreatic mass does not show clinico-radiological features typical of common pancreatic neoplasms, XGP should be considered for a differential diagnosis.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Case of Xanthogranulomatous Sialadenitis with Facial Palsy Mimicking Malignancy
Sang Hyun Kim, Sun Woo Kim, Sang Hyuk Lee
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(6):422-428. doi: 10.3342/kjorl-hns.2020.00388.
Reference
-
1. Kwak JE, Kim HS, Joo M, Chang SH, Shim SH, Chi JG, Cho IR. Combined xanthogranulomatous urachitis and bullous cystitis: a case report. Korean J Pathol. 2008. 42:41–44.2. Houston JP, Collins MC, Cameron I, Reed MW, Parsons MA, Roberts KM. Xanthogranulomatous cholecystitis. Br J Surg. 1994. 81:1030–1032.3. Choi YH, Choi WH, Han SY, Han KH, Kim HS. A case of bilateral xanthogranulomatous pyelonephritis with renal failure. Korean J Nephrol. 2008. 27:137–140.4. Ueno T, Hamanaka Y, Nishihara K, Nishida M, Nishikawa M, Kawabata A, Yamamoto S, Tsurumi M, Suzuki T. Xanthogranulomatous change appearing in the pancreas cyst wall. Pancreas. 1993. 8:649–651.5. Iyer VK, Aggarwal S, Mathur M. Xanthogranulomatous pancreatitis: mass lesion of the pancreas simulating pancreatic carcinoma--a report of two cases. Indian J Pathol Microbiol. 2004. 47:36–38.6. Kamitani T, Nishimiya M, Takahashi N, Shida Y, Hasuo K, Koizuka H. Xanthogranulomatous pancreatitis associated with intraductal papillary mucinous tumor. AJR Am J Roentgenol. 2005. 185:704–707.7. Okabayashi T, Nishimori I, Kobayashi M, Sugimoto T, Kohsaki T, Okamoto K, Ito S, Moriki T, Araki K, Onishi S. Xanthogranulomatous pancreatic abscess secondary to acute pancreatitis: two case reports. Hepatogastroenterology. 2007. 54:1648–1651.8. Shima Y, Saisaka Y, Furukita Y, Nishimura T, Horimi T, Nakamura T, Tanaka K, Shibuya Y, Ozaki K, Fukui Y, Hamada M, Nishioka Y, Okabayashi T, Taniki T, Morita S, Iwata J. Resected xanthogranulomatous pancreatitis. J Hepatobiliary Pancreat Surg. 2008. 15:240–242.9. Iso Y, Tagaya N, Kita J, Sawada T, Kubota K. Xanthogranulomatous lesion of the pancreas mimicking pancreatic cancer. Med Sci Monit. 2008. 14:CS130–CS133.10. Ikeura T, Takaoka M, Shimatani M, Koyabu M, Kusuda T, Suzuki R, Sumimoto K, Okazaki K. Xanthogranulomatous inflammation of the peripancreatic region mimicking pancreatic cystic neoplasm. Intern Med. 2009. 48:1881–1884.11. Uguz A, Yakan S, Gurcu B, Yilmaz F, Ilter T, Coker A. Xanthogranulomatous pancreatitis treated by duodenum-preserving pancreatic head resection. Hepatobiliary Pancreat Dis Int. 2010. 9:216–218.12. Kang BW, Kim JW, Jo JC, Lee SS, Seo DW, Lee SK, Kim MH. A case of xanthogranulomatous pancreatitis. Korean J Med. 2007. 72:Suppl 2. S171–S174.13. Kim YN, Park SY, Kim YK, Moon WS. Xanthogranulomatous pancreatitis combined with intraductal papillary mucinous carcinoma in situ. J Korean Med Sci. 2010. 25:1814–1817.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Xanthogranulomatous pancreatitis mimicking potentially malignant pancreatic neoplasm: report of a case
- Xanthogranulomatous Pancreatitis Mimicking a Pancreatic Cancer on CT and MRI: a Case Report and Literature Review
- Xanthogranulomatous Osteomyelitis Presenting as a Subacute Infectious Condition in the Fibula of a Young Female
- Two Cases of Xanthogranulomatous Pyelonephritis
- A Case of Xanthogranulomatous Pyelonephritis which was Confused with Renal Pelvic Tumor