J Korean Med Sci.
2011 Apr;26(4):474-481. 10.3346/jkms.2011.26.4.474.
Tissue Plasminogen Activator and Plasminogen Activator Inhibitor-1 Levels in Patients with Acute Paraquat Intoxication
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Soonchunhyang University, Cheonan, Korea. syhong@sch.ac.kr
- KMID: 1777876
- DOI: http://doi.org/10.3346/jkms.2011.26.4.474
Abstract
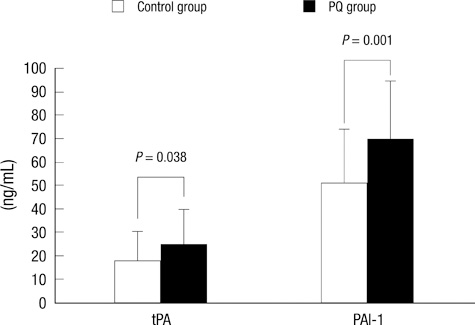
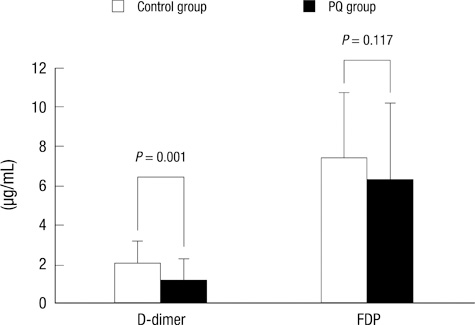
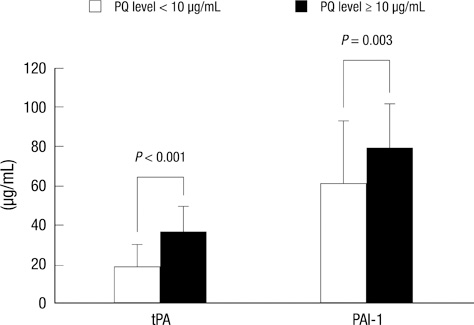
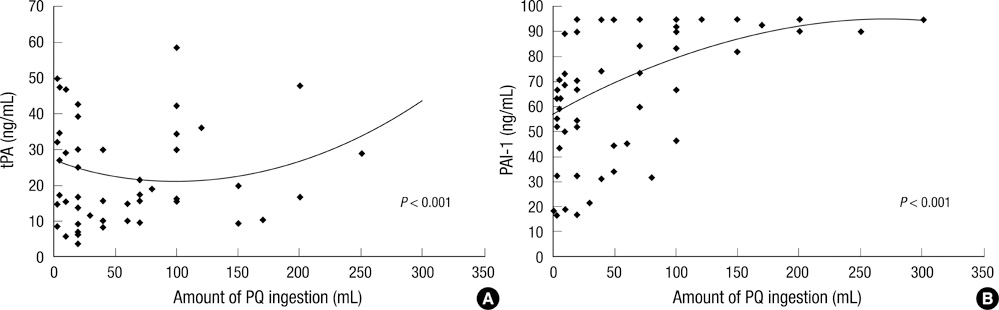
- To investigate the effects of reactive oxygen species (ROS) on tissue plasminogen activator (tPA) and plasminogen activator inhibitor-1 (PAI-1) plasma levels, and their possible implications on clinical outcome, we measured tPA and PAI-1 levels in 101 patients with acute paraquat (PQ) intoxication. The control group consisted of patients who ingested non-PQ pesticides during the same period. tPA and PAI-1 levels were higher in the PQ group than in the controls. PQ levels were significantly correlated with ingested amount, timelag to hospital, tPA level, and hospitalization duration. tPA levels were correlated with PAI-1, fibrin degradation product (FDP), and D-dimer. D-dimer levels were lower in the PQ group than in the controls. Univariate analysis indicated the following significant determinants of death: age, ingested amount, PQ level, timelag to hospital, serum creatinine, lipase, pH, pCO2, HCO3-, WBC, FDP, PAI-1, and tPA. However, multivariate analysis indicated that only PQ level was significant independent factor predicting death. In conclusion, tPA and PAI-1 levels were higher, while D-dimer levels were lower in the PQ group than in the controls, implying that ROS stimulate tPA and PAI-1, but PAI-1 activity overrides tPA activity in this setting. Decreased fibrinolytic activity appears to be one of the clinical characteristics of acute PQ intoxication.
Keyword
MeSH Terms
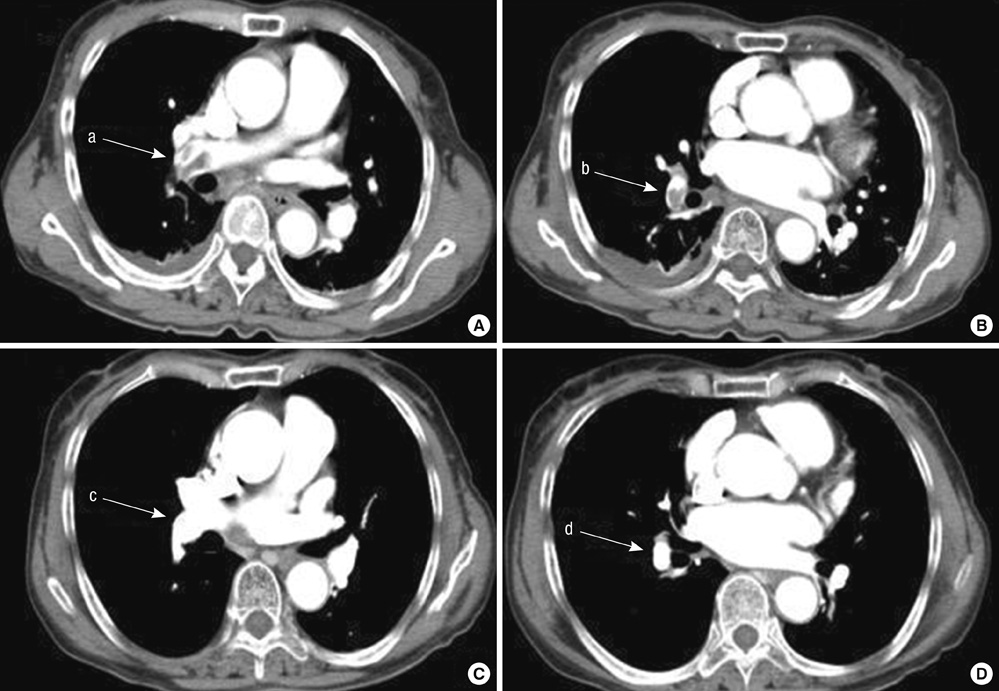
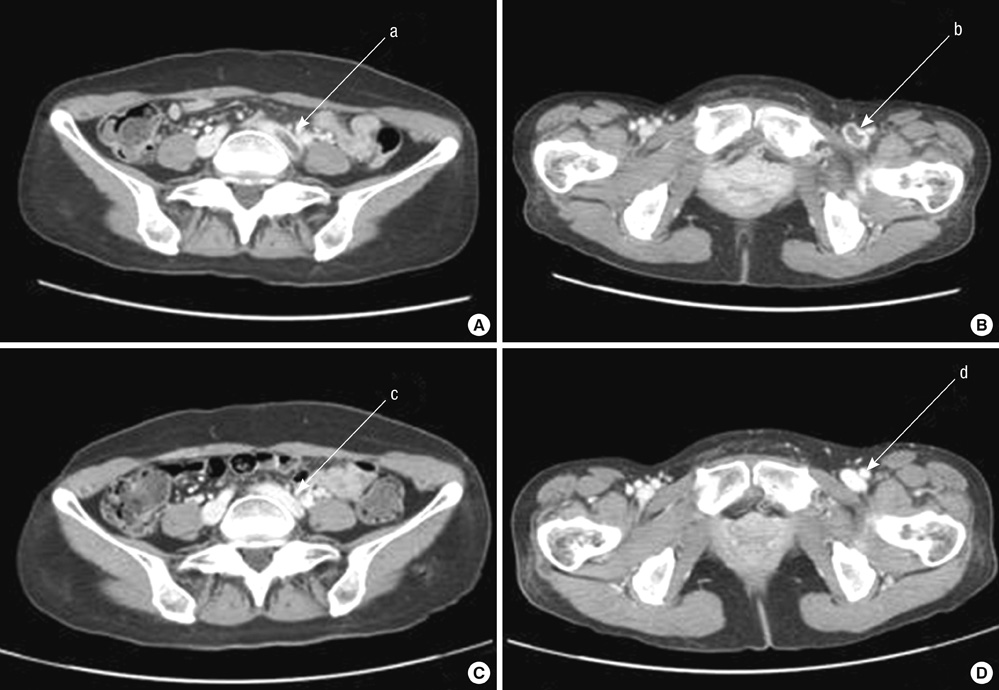
Figure
Reference
-
1. Collen D, Lijnen HR. Tissue-type plasminogen activator: a historical perspective and personal account. J Thromb Haemost. 2004. 2:541–546.2. Zorio E, Gilabert-Estellés J, España F, Ramón LA, Cosín R, Estellés A. Fibrinolysis: the key to new pathogenetic mechanisms. Curr Med Chem. 2008. 15:923–929.3. Nagamine Y. Transcriptional regulation of the plasminogen activator inhibitor type 1 with an emphasis on negative regulation. Thromb Haemost. 2008. 100:1007–1013.4. Wu WS. The signaling mechanism of ROS in tumor progression. Cancer Metastasis Rev. 2006. 25:695–705.5. Nusbaum C, Mikkelsen TS, Zody MC, Asakawa S, Taudien S, Garber M, Kodira CD, Schueler MG, Shimizu A, Whittaker CA, Chang JL, Cuomo CA, Dewar K, FitzGerald MG, Yang X, Allen NR, Anderson S, Asakawa T, Blechschmidt K, Bloom T, Borowsky ML, Butler J, Cook A, Corum B, DeArellano K, DeCaprio D, Dooley KT, Dorris L 3rd, Engels R, Glöckner G, Hafez N, Hagopian DS, Hall JL, Ishikawa SK, Jaffe DB, Kamat A, Kudoh J, Lehmann R, Lokitsang T, Macdonald P, Major JE, Matthews CD, Mauceli E, Menzel U, Mihalev AH, Minoshima S, Murayama Y, Naylor JW, Nicol R, Nguyen C, O'Leary SB, O'Neill K, Parker SC, Polley A, Raymond CK, Reichwald K, Rodriguez J, Sasaki T, Schilhabel M, Siddiqui R, Smith CL, Sneddon TP, Talamas JA, Tenzin P, Topham K, Venkataraman V, Wen G, Yamazaki S, Young SK, Zeng Q, Zimmer AR, Rosenthal A, Birren BW, Platzer M, Shimizu N, Lander ES. DNA sequence and analysis of human chromosome 8. Nature. 2006. 439:331–335.6. Shatos MA, Doherty JM, Stump DC, Thompson EA, Collen D. Oxygen radicals generated during anoxia followed by reoxygenation reduce the synthesis of tissue-type plasminogen activator and plasminogen activator inhibitor-1 in human endothelial cell culture. J Biol Chem. 1990. 265:20443–20448.7. Eberhardt W, Beck KF, Pfeilschifter J. Cytokine-induced expression of tPA is differentially modulated by NO and ROS in rat mesangial cells. Kidney Int. 2002. 61:20–30.8. Feng YH, Hart G. In vitro oxidative damage to tissue-type plasminogen activator: a selective modification of the biological functions. Cardiovasc Res. 1995. 30:255–261.9. Van Guilder GP, Hoetzer GL, Greiner JJ, Stauffer BL, DeSouza CA. Acute and chronic effects of vitamin C on endothelial fibrinolytic function in overweight and obese adult humans. J Physiol. 2008. 586:3525–3535.10. Dellas C, Loskutoff DJ. Historical analysis of PAI-1 from its discovery to its potential role in cell motility and disease. Thromb Haemost. 2005. 93:631–640.11. Asselbergs FW, Pattin K, Snieder H, Hillege HL, van Gilst WH, Moore JH. Genetic architecture of tissue-type plasminogen activator and plasminogen activator inhibitor-1. Semin Thromb Hemost. 2008. 34:562–568.12. Kruithof EK. Regulation of plasminogen activator inhibitor type 1 gene expression by inflammatory mediators and statins. Thromb Haemost. 2008. 100:969–975.13. Seok SJ, Gil HW, Jeong DS, Yang JO, Lee EY, Hong SY. Paraquat intoxication in subjects who attempt suicide: why they chose paraquat. Korean J Intern Med. 2009. 24:247–251.14. Lee KH, Gil HW, Kim YT, Yang JO, Lee EY, Hong SY. Marked recovery from paraquat-induced lung injury during long-term follow-up. Korean J Intern Med. 2009. 24:95–100.15. Gil HW, Kang MS, Yang JO, Lee EY, Hong SY. Association between plasma paraquat level and outcome of paraquat poisoning in 375 paraquat poisoning patients. Clin Toxicol (Phila). 2008. 46:515–518.16. Kim YT, Jou SS, Lee HS, Gil HW, Yang JO, Lee EY, Hong SY. The area of ground glass opacities of the lungs as a predictive factor in acute paraquat intoxication. J Korean Med Sci. 2009. 24:636–640.17. Hong SY, Yang JO, Lee EY, Lee ZW. Effects of N-acetyl-L-cysteine and glutathione on antioxidant status of human serum and 3T3 fibroblasts. J Korean Med Sci. 2003. 18:649–654.18. Collen D, Lijnen HR. Thrombolytic agents. Thromb Haemost. 2005. 93:627–630.19. Murray V, Norrving B, Sandercock PA, Terént A, Wardlaw JM, Wester P. The molecular basis of thrombolysis and its clinical application in stroke. J Intern Med. 2010. 267:191–208.20. Lijfering WM, Rosendaal FR, Cannegieter SC. Risk factors for venous thrombosis- current understanding from an epidemiological point of view. Br J Haematol. 2010. 149:824–833.21. Kahn SR, Shrier I, Kearon C. Physical activity in patients with deep venous thrombosis: a systematic review. Thromb Res. 2008. 122:763–773.22. Ortel TL. Acquired thrombotic risk factors in the critical care setting. Crit Care Med. 2010. 38:2 Suppl. S43–S50.23. Gil HW, Kim SJ, Yang JO, Lee EY, Hong SY. Clinical outcome of hemoperfusion in poisoned patients. Blood Purif. 2010. 30:84–88.24. Gil HW, Seok SJ, Jeong DS, Yang JO, Lee EY, Hong SY. Plasma level of malondialdehyde in the cases of acute paraquat intoxication. Clin Toxicol (Phila). 2010. 48:149–152.25. Kim JH, Gil HW, Yang JO, Lee EY, Hong SY. Effect of glutathione administration on serum levels of reactive oxygen metabolites in patients with paraquat intoxication: a pilot study. Korean J Intern Med. 2010. 25:282–287.26. Thachil J, Fitzmaurice DA, Toh CH. Appropriate use of D-dimer in hospital patients. Am J Med. 2010. 123:17–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of immune-mediated vascular injury on the coagulation- regulatory mechanism of the human endothelial cells; changes of tissue-type plasminogen activator, plasminogen activator inhibitor- 1 and von Willebrand factor
- Urokinase-type plasminogen activator receptor in IgA nephropathy
- Expression of type I plasminogen activator inhibitor in renal tissue in murine lupus
- Effects of the dosing regimen of tissue-type plasminogen activator on blood coagulation system in experimental pulmonary embolism
- Studies on Fibrinolytic System Behavior in Women with Polycystic Ovary Syndrome