J Korean Med Sci.
2013 Oct;28(10):1449-1453. 10.3346/jkms.2013.28.10.1449.
Status of Primary Liver Cancer Found through Routine Health Check-up
- Affiliations
-
- 1Department of Internal Medicine, Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, Korea. dr1004@snu.ac.kr
- KMID: 1777680
- DOI: http://doi.org/10.3346/jkms.2013.28.10.1449
Abstract
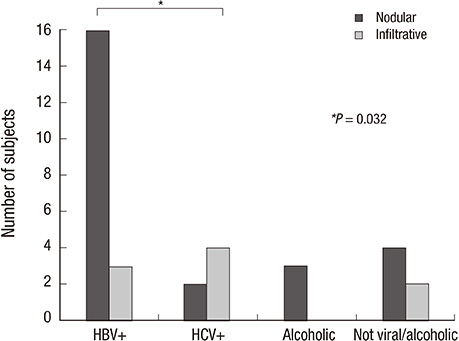
- This study aimed to investigate the status of primary liver cancers found through a routine health check-up. The data of subjects who were diagnosed with primary liver cancer for the first time through a routine health check-up during a period of 8-yr were analyzed. Primary liver cancers were detected for the first time in 34 subjects among 91,219 routine health check-up subjects. Only 11.8% of primary liver cancer subjects had been under previous surveillance. Of them, 55.8% were positive for HBsAg, 17.7% were positive for anti-HCV, and 8.8% were heavy alcohol comsumers. However, 17.7% of the subjects were neither heavy alcohol consumers nor positive for both HBsAg and anti-HCV. Of the subjects, 50.0% had a single nodular tumor, 23.5% had multi-nodular tumors, and 26.5% had an infiltrative tumor. A routine health check-up may provide beneficial opportunities to detect a liver cancer in a very early stage. It is beneficial to start surveillance in high-risk subjects for liver cancer or to detect any liver cancer in subjects without risk factors of chronic viral hepatitis or heavy alcohol consumption.
MeSH Terms
Figure
Reference
-
1. Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010; 4:439–474.2. European Association for the Study of the Liver. European Organisation for Research and treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943.3. De Lope CR, Tremosini S, Forner A, Reig M, Bruix J. Management of HCC. J Hepatol. 2012; 56:S75–S87.4. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022.5. Bae SY, Choi MS, Gwak GY, Paik YH, Lee JH, Koh KC, Paik SW, Yoo BC. Comparison of usefulness of clinical diagnostic criteria for hepatocellular carcinoma in a hepatitis B endemic area. Clin Mol Hepatol. 2012; 18:185–194.6. Statistics Korea. Korean Statistical Information Service by Statistics Korea. accessed on 10 April 2013. Available at http://kosis.kr/abroad/abroad_01List.jsp?parentId=D.7. Song IH, Kim KS. Current status of liver diseases in Korea: hepatocellular carcinoma. Korean J Hepatol. 2009; 15:S50–S59.8. National cancer control programs in Korea. J Korean Med Sci. 2007; 22:S3–S4.9. Lee JJ, Park SK, Kwon OS, Won IS, Kim DK, Jung YK, Ku YS, Kim YS, Choi DJ, Kim JH. Genetic polymorphism at codon 10 of the transforming growth factor-beta1 gene in patients with alcoholic liver cirrhosis. Korean J Hepatol. 2011; 17:37–43.10. Korean Liver Cancer Study Group and National Cancer Center, Korea. Practice guidelines for management of hepatocellular carcinoma 2009. Korean J Hepatol. 2009; 15:391–423.11. Lee J, Lee JM, Yoon JH, Lee JY, Kim SH, Lee JE, Han JK, Choi BI. Percutaneous radiofrequency ablation with multiple electrodes for medium-sized hepatocellular carcinomas. Korean J Radiol. 2012; 13:34–43.12. Jang ES, Yoon JH, Chung JW, Cho EJ, Yu SJ, Lee JH, Kim YJ, Lee HS, Kim CY. Survival of infiltrative hepatocellular carcinoma patients with preserved hepatic function after treatment with transarterial chemoembolization. J Cancer Res Clin Oncol. 2013; 139:635–643.13. Cho YB, Lee KU, Suh KS, Kim YJ, Yoon JH, Lee HS, Hahn S, Park BJ. Hepatic resection compared to percutaneous ethanol injection for small hepatocellular carcinoma using propensity score matching. J Gastroenterol Hepatol. 2007; 22:1643–1649.14. Stravitz RT, Heuman DM, Chand N, Sterling RK, Shiffman ML, Luketic VA, Sanyal AJ, Habib A, Mihas AA, Giles HC, et al. Surveillance for hepatocellular carcinoma in patients with cirrhosis improves outcome. Am J Med. 2008; 121:119–126.15. Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004; 127:S5–S16.16. Lee HS, Han CJ, Kim CY. Predominant etiologic association of hepatitis C virus with hepatocellular carcinoma compared with hepatitis B virus in elderly patients in a hepatitis B-endemic area. Cancer. 1993; 72:2564–2567.17. Umemura T, Ichijo T, Yoshizawa K, Tanaka E, Kiyosawa K. Epidemiology of hepatocellular carcinoma in Japan. J Gastroenterol. 2009; 44:102–107.18. Jung SH, Kim BH, Joung YH, Han YS, Lee BH, Dong SH, Kim HJ, Chang YW, Lee JI, Chang R. Clinical features of hepatocellular carcinoma in the 1990s. Korean J Gastroenterol. 2003; 42:322–329.19. Purohit V, Rapaka R, Kwon OS, Song BJ. Roles of alcohol and tobacco exposure in the development of hepatocellular carcinoma. Life Sci. 2013; 92:3–9.20. Arase Y, Kobayashi M, Suzuki F, Suzuki Y, Kawamura Y, Akuta N, Kobayashi M, Sezaki H, Saito S, Hosaka T, et al. Effect of type 2 diabetes on risk for malignancies includes hepatocellular carcinoma in chronic hepatitis C. Hepatology. 2013; 57:964–973.21. Wang P, Kang D, Cao W, Wang Y, Liu Z. Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2012; 28:109–122.22. Wang C, Wang X, Gong G, Ben Q, Qiu W, Chen Y, Li G, Wang L. Increased risk of hepatocellular carcinoma in patients with diabetes mellitus: a systematic review and meta-analysis of cohort studies. Int J Cancer. 2012; 130:1639–1648.23. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309:71–82.24. Schlesinger S, Aleksandrova K, Pischon T, Fedirko V, Jenab M, Trepo E, Boffetta P, Dahm CC, Overvad K, Tjønneland A, et al. Abdominal obesity, weight gain during adulthood and risk of liver and biliary tract cancer in a European cohort. Int J Cancer. 2013; 132:645–657.25. Tanaka K, Tsuji I, Tamakoshi A, Matsuo K, Ito H, Wakai K, Nagata C, Mizoue T, Sasazuki S, Inoue M, et al. Obesity and liver cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol. 2012; 42:212–221.26. Gouas D, Shi H, Hainaut P. The aflatoxin-induced TP53 mutation at codon 249 (R249S): biomarker of exposure, early detection and target for therapy. Cancer Lett. 2009; 286:29–37.27. Sherman M. The resurrection of alphafetoprotein. J Hepatol. 2010; 52:939–940.28. Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS, Lee WJ, Park SJ, Hong EK, Kim CM. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2008; 23:467–473.29. Oliveri RS, Wetterslev J, Gluud C. Hepatocellular carcinoma. Lancet. 2012; 380:470.30. Chua TC, Liauw W, Saxena A, Chu F, Glenn D, Chai A, Morris DL. Systematic review of neoadjuvant transarterial chemoembolization for resectable hepatocellular carcinoma. Liver Int. 2010; 30:166–174.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association Chronic Liver Diseases with Health Related Behaviors in South Korea
- Asymptomatic Gastric Band Erosion Detected during Routine Gastroduodenoscopy
- A Study of Esophageal Cancer Detected by Screening Upper Endoscopy for a Routine Health Check-up
- Clinical Features of Gastric Cancer Patients with a Second Primary Cancer
- Current Status of Research on Liver Cancer in Korea