Yonsei Med J.
2013 Jan;54(1):160-165. 10.3349/ymj.2013.54.1.160.
Prevalence and Risk Factors of Esophageal Candidiasis in Healthy Individuals: A Single Center Experience in Korea
- Affiliations
-
- 1Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University-Seoul, Graduate School of Medicine, Goyang, Korea. limyj@dongguk.ac.kr
- 2Department of Biostatistics, Dongguk University Ilsan Hospital, Dongguk University-Seoul, Graduate School of Medicine, Goyang, Korea.
- 3Department of Pathology, Dongguk University Ilsan Hospital, Dongguk University-Seoul, Graduate School of Medicine, Goyang, Korea.
- KMID: 1776932
- DOI: http://doi.org/10.3349/ymj.2013.54.1.160
Abstract
- PURPOSE
Esophageal candidiasis (EC) is the most frequent opportunistic fungal infection in immunocompromised host. However, we have found EC in healthy individuals through esophagogastroduodenoscopy (EGD). The aim of this study was to determine the prevalence and risk factors for EC in healthy individuals.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of 281 patients who had been incidentally diagnosed with EC. We also conducted age and sex matched case control study to identify the risk factor for EC.
RESULTS
The prevalence of EC was 0.32% (281/88125). The most common coexisting EGD finding was reflux esophagitis (49/281, 17.4%). An antifungal agent was prescribed in about half of EC, 139 cases (49.5%). Follow-up EGD was undertaken in 83 cases (29.5%) and 20 cases of candidiasis was persistently found. Case control study revealed EC were more often found in user of antibiotics (p=0.015), corticosteroids (p=0.002) and herb medication (p=0.006) as well as heavy drinking (p<0.001).
CONCLUSION
The prevalence of EC was 0.32% (281/88125) in Korea. Use of antibiotics, corticosteroids and herb as well as heavy drinking were significant risk factors for EC in healthy individuals.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones/therapeutic use
Adult
Aged
Alcohol Drinking
Anti-Bacterial Agents/therapeutic use
Antifungal Agents/pharmacology
Candidiasis/*diagnosis/epidemiology
Case-Control Studies
Esophageal Diseases/*diagnosis/epidemiology
Esophagitis, Peptic/complications/diagnosis
Female
Humans
Immunocompromised Host
Male
Middle Aged
Plant Preparations/therapeutic use
Prevalence
Republic of Korea
Retrospective Studies
Risk Factors
Adrenal Cortex Hormones
Anti-Bacterial Agents
Antifungal Agents
Plant Preparations
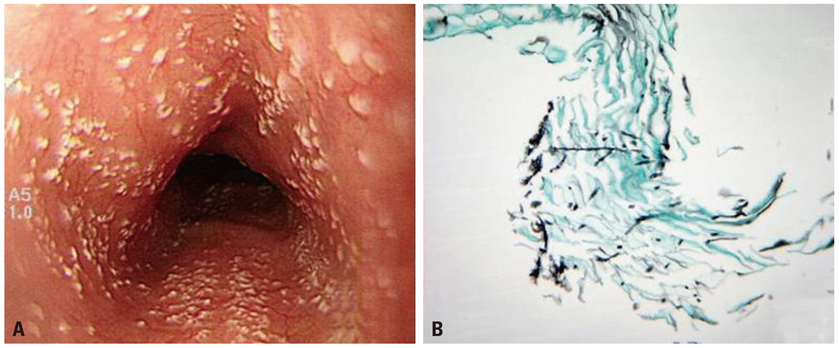
Figure
Reference
-
1. Laine L, Bonacini M. Esophageal disease in human immunodeficiency virus infection. Arch Intern Med. 1994. 154:1577–1582.
Article2. Thapa BR, Kumar L. Candida esophagitis after antibiotic use. Indian J Pediatr. 1989. 56:296–299.
Article3. Kochhar R, Talwar P, Singh S, Mehta SK. Invasive candidiasis following cimetidine therapy. Am J Gastroenterol. 1988. 83:102–103.4. Karmeli Y, Stalnikowitz R, Eliakim R, Rahav G. Conventional dose of omeprazole alters gastric flora. Dig Dis Sci. 1995. 40:2070–2073.
Article5. Weerasuriya N, Snape J. Oesophageal candidiasis in elderly patients: risk factors, prevention and management. Drugs Aging. 2008. 25:119–130.6. Baehr PH, McDonald GB. Esophageal infections: risk factors, presentation, diagnosis, and treatment. Gastroenterology. 1994. 106:509–532.
Article7. Simon MR, Houser WL, Smith KA, Long PM. Esophageal candidiasis as a complication of inhaled corticosteroids. Ann Allergy Asthma Immunol. 1997. 79:333–338.
Article8. Phaosawasdi K, Rice P, Lee B. Primary and secondary Candida esophagitis. IMJ Ill Med J. 1986. 169:361–365.9. Mathieson R, Dutta SK. Candida esophagitis. Dig Dis Sci. 1983. 28:365–370.
Article10. Hoshika K, Iida M, Mine H. Esophageal Candida infection and adherence mechanisms in the nonimmunocompromised rabbit. J Gastroenterol. 1996. 31:307–313.
Article11. Vermeersch B, Rysselaere M, Dekeyser K, Rasquin K, De Vos M, Elewaut A, et al. Fungal colonization of the esophagus. Am J Gastroenterol. 1989. 84:1079–1083.12. Underwood JA, Williams JW, Keate RF. Clinical findings and risk factors for Candida esophagitis in outpatients. Dis Esophagus. 2003. 16:66–69.
Article13. Naito Y, Yoshikawa T, Oyamada H, Tainaka K, Morita Y, Kogawa T, et al. Esophageal candidiasis. Gastroenterol Jpn. 1988. 23:363–370.
Article14. Tamura Y, Araki A, Chiba Y, Ishimaru Y, Ishimaru Y, Horiuchi T, et al. A case of type 2 diabetes mellitus in an elderly patient with rapid attenuation of insulin secretion that resembled fulminant type 1 DM but with incomplete beta cell damage. Endocr J. 2006. 53:633–637.
Article15. Rex JH, Walsh TJ, Sobel JD, Filler SG, Pappas PG, Dismukes WE, et al. Infectious Diseases Society of America. Practice guidelines for the treatment of candidiasis. Clin Infect Dis. 2000. 30:662–678.
Article16. Vazquez JA. Invasive oesophageal candidiasis: current and developing treatment options. Drugs. 2003. 63:971–989.17. Cascio A, Barone M, Micali V, Iaria C, Delfino D, David A, et al. On a fatal case of Candida krusei pleural empyema in a pregnant woman with spontaneous esophagus perforation. Mycopathologia. 2010. 169:451–455.
Article18. Tran HA, Vincent JM, Slavin MA, Grigg A. Esophageal perforation secondary to angio-invasive Candida glabrata following hemopoietic stem cell transplantation. Clin Microbiol Infect. 2003. 9:1215–1218.
Article19. Al-Shawwa B, D'Andrea L, Quintero D. Candida esophageal perforation and esophagopleural fistula: a case report. J Med Case Rep. 2008. 2:209.
Article20. Kanakala V, Lamb CA, Haigh C, Stirling RW, Attwood SE. The diagnosis of primary eosinophilic oesophagitis in adults: missed or misinterpreted? Eur J Gastroenterol Hepatol. 2010. 22:848–855.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Candidiasis and Early Childhood Caries : Analysis Using Healthcare Big Data
- A Case of Esophageal Candidiasis in a Healthy Child
- A Case of Aggravated Esophageal Candidiasis and Gastric Yeast Bezoar Formation following Gastric Outlet Obstruction due to Duodenal Stenosis
- A case of esophageal candidiasis caused by inhaled corticosteroid
- Recurrent Esophageal Stricture Caused by Candidiasis in an HIV-Infected Patient