Korean J Radiol.
2014 Aug;15(4):423-429. 10.3348/kjr.2014.15.4.423.
Extra-Mammary Findings Detected on Breast Magnetic Resonance Imaging: A Pictorial Essay
- Affiliations
-
- 1Cancer Prevention & Detection Center, National Cancer Center, Goyang 410-769, Korea.
- 2Department of Radiology, National Cancer Center, Goyang 410-769, Korea. kokr@ncc.re.kr
- KMID: 1731044
- DOI: http://doi.org/10.3348/kjr.2014.15.4.423
Abstract
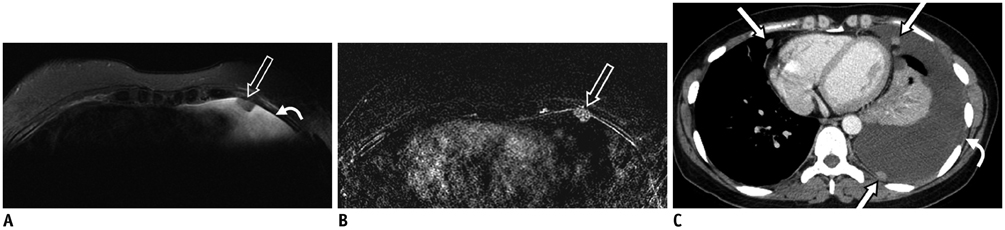
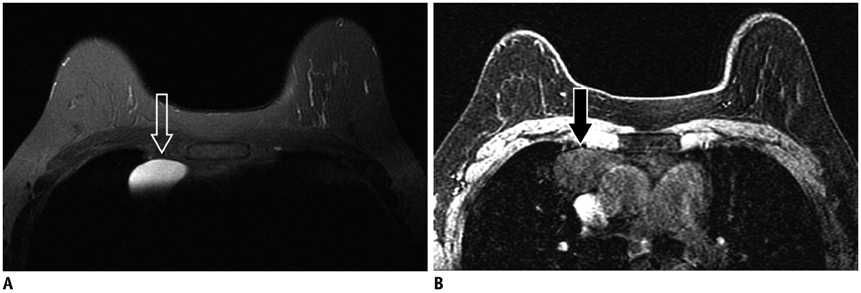
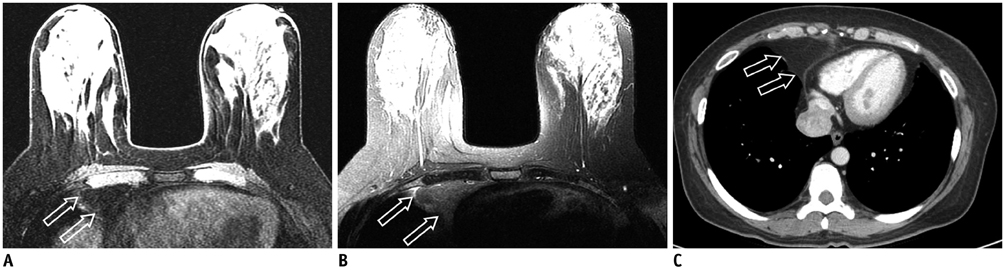
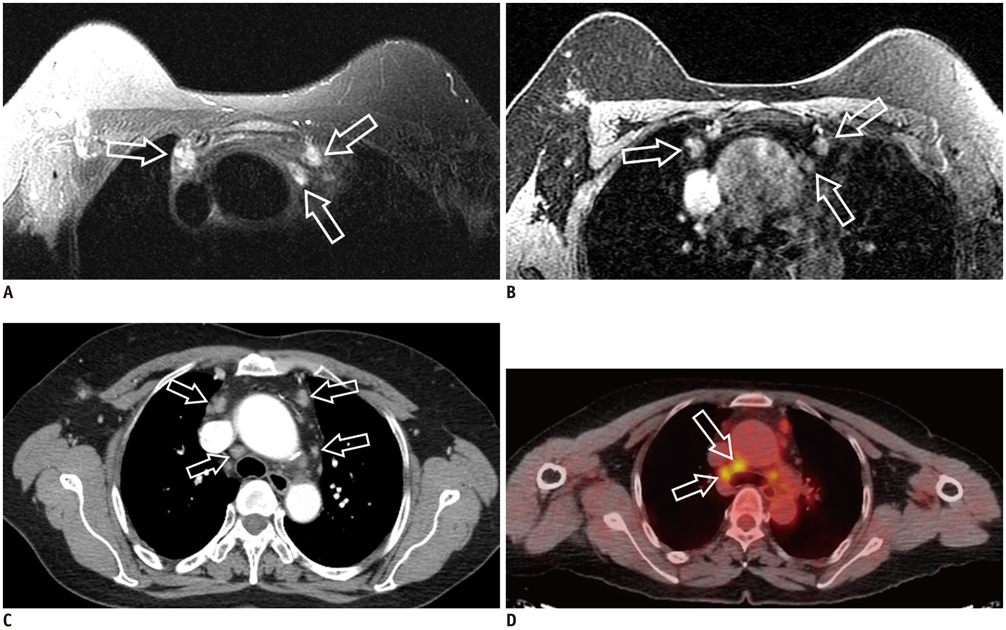
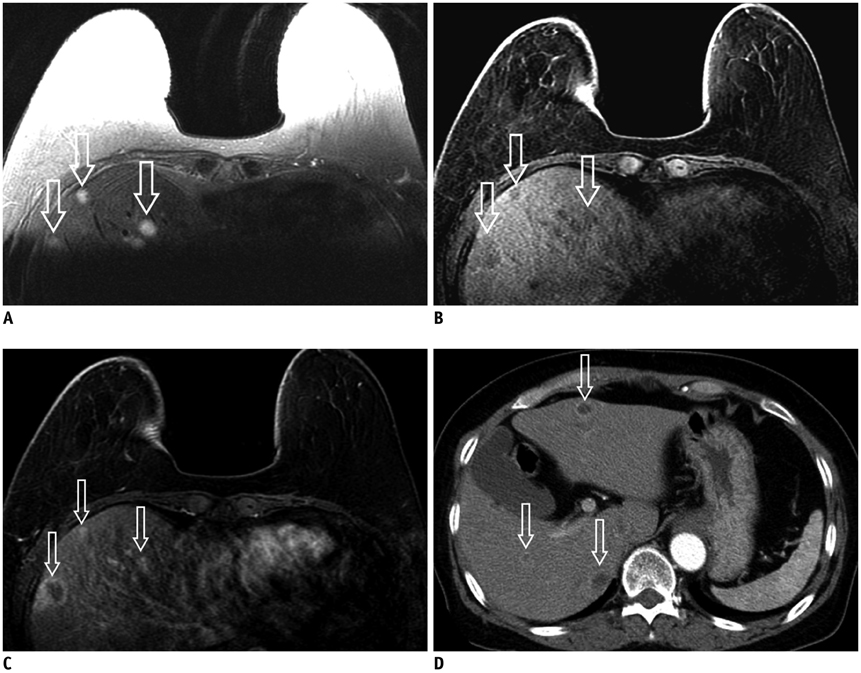
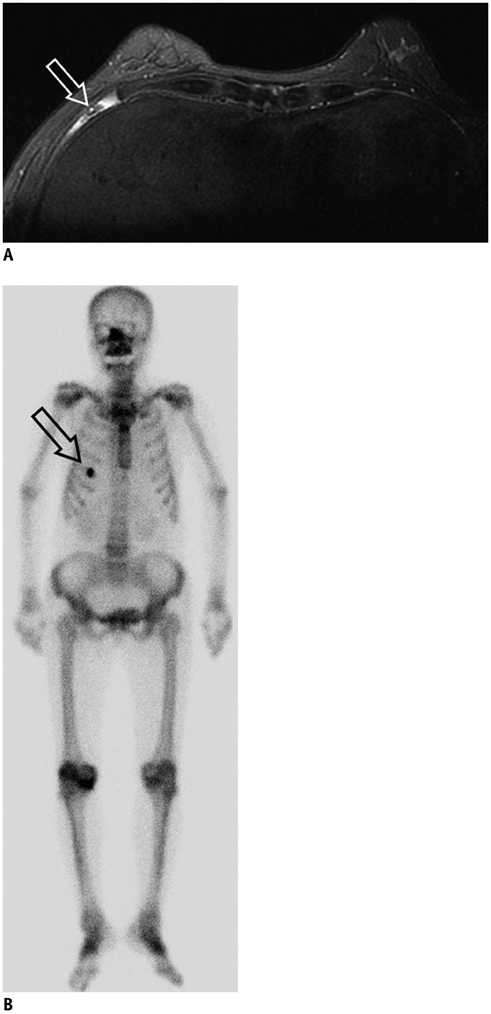
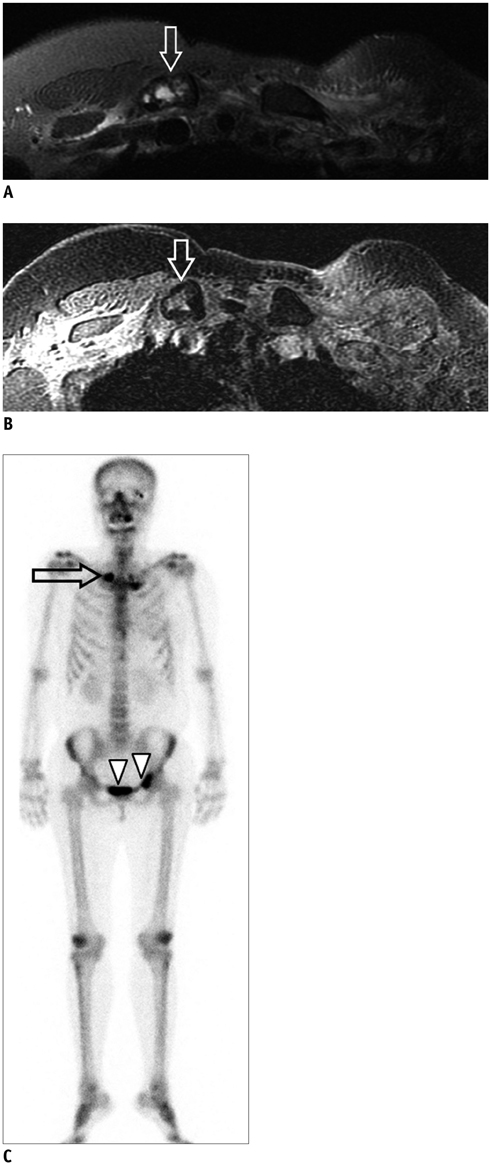
- Magnetic resonance imaging (MRI) of the breast is used for various indications. Contrary to computed tomography as a staging tool, breast MRI focuses on the breast parenchyma and axilla. In spite of narrow field of view, many structures such as the anterior portion of the lungs, mediastinum, bony structures and the liver are included which should not be neglected because the abnormalities detected on the above structures may influence the staging and provide a clue to systemic metastasis, which results in the change of treatment strategy. The purpose of this pictorial essay was to review the unexpected extra-mammary findings seen on the preoperative breast MRI.
Keyword
MeSH Terms
Figure
Reference
-
1. Vassiou K, Kanavou T, Vlychou M, Poultsidi A, Athanasiou E, Arvanitis DL, et al. Characterization of breast lesions with CE-MR multimodal morphological and kinetic analysis: comparison with conventional mammography and high-resolution ultrasound. Eur J Radiol. 2009; 70:69–76.2. Rinaldi P, Costantini M, Belli P, Giuliani M, Bufi E, Fubelli R, et al. Extra-mammary findings in breast MRI. Eur Radiol. 2011; 21:2268–2276.3. Rausch DR. Spectrum of extra-mammary findings on breast MRI: a pictorial review. Breast J. 2008; 14:592–594.4. Chang EY, Johnson W, Karamlou K, Khaki A, Komanapalli C, Walts D, et al. The evaluation and treatment implications of isolated pulmonary nodules in patients with a recent history of breast cancer. Am J Surg. 2006; 191:641–645.5. Rashid OM, Takabe K. The evolution of the role of surgery in the management of breast cancer lung metastasis. J Thorac Dis. 2012; 4:420–424.6. MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005; 237:395–400.7. Laurent F, Latrabe V, Lecesne R, Zennaro H, Airaud JY, Rauturier JF, et al. Mediastinal masses: diagnostic approach. Eur Radiol. 1998; 8:1148–1159.8. Schwartz LH, Gandras EJ, Colangelo SM, Ercolani MC, Panicek DM. Prevalence and importance of small hepatic lesions found at CT in patients with cancer. Radiology. 1999; 210:71–74.9. Hamm B, Thoeni RF, Gould RG, Bernardino ME, Lüning M, Saini S, et al. Focal liver lesions: characterization with nonenhanced and dynamic contrast material-enhanced MR imaging. Radiology. 1994; 190:417–423.10. Major PP, Cook RJ, Lipton A, Smith MR, Terpos E, Coleman RE. Natural history of malignant bone disease in breast cancer and the use of cumulative mean functions to measure skeletal morbidity. BMC Cancer. 2009; 9:272.11. Costelloe CM, Rohren EM, Madewell JE, Hamaoka T, Theriault RL, Yu TK, et al. Imaging bone metastases in breast cancer: techniques and recommendations for diagnosis. Lancet Oncol. 2009; 10:606–614.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging Features of Inflammatory Breast Disorders: A Pictorial Essay
- Imaging Features of the Mesenchymal Tumors of the Breast according to WHO Classification: A Pictorial Essay
- Tips for finding magnetic resonance imaging-detected suspicious breast lesions using second-look ultrasonography: a pictorial essay
- Imaging Spectrum of Augmented Breast and Post-Mastectomy Reconstructed Breast with Common Complications: A Pictorial Essay
- Incidental Extramammary Findings on Preoperative Breast MRI in Breast Cancer Patients: A Pictorial Essay