Korean J Gastroenterol.
2014 Feb;63(2):129-133. 10.4166/kjg.2014.63.2.129.
Synchronous Malignant Intraductal Papillary Mucinous Neoplasms of the Bile Duct and Pancreas Requiring Left Hepatectomy and Total Pancreatectomy
- Affiliations
-
- 1Hepatobiliary Surgery and Liver Transplantation, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sglee2@amc.seoul.kr
- 2Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Diagnostic Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1730921
- DOI: http://doi.org/10.4166/kjg.2014.63.2.129
Abstract
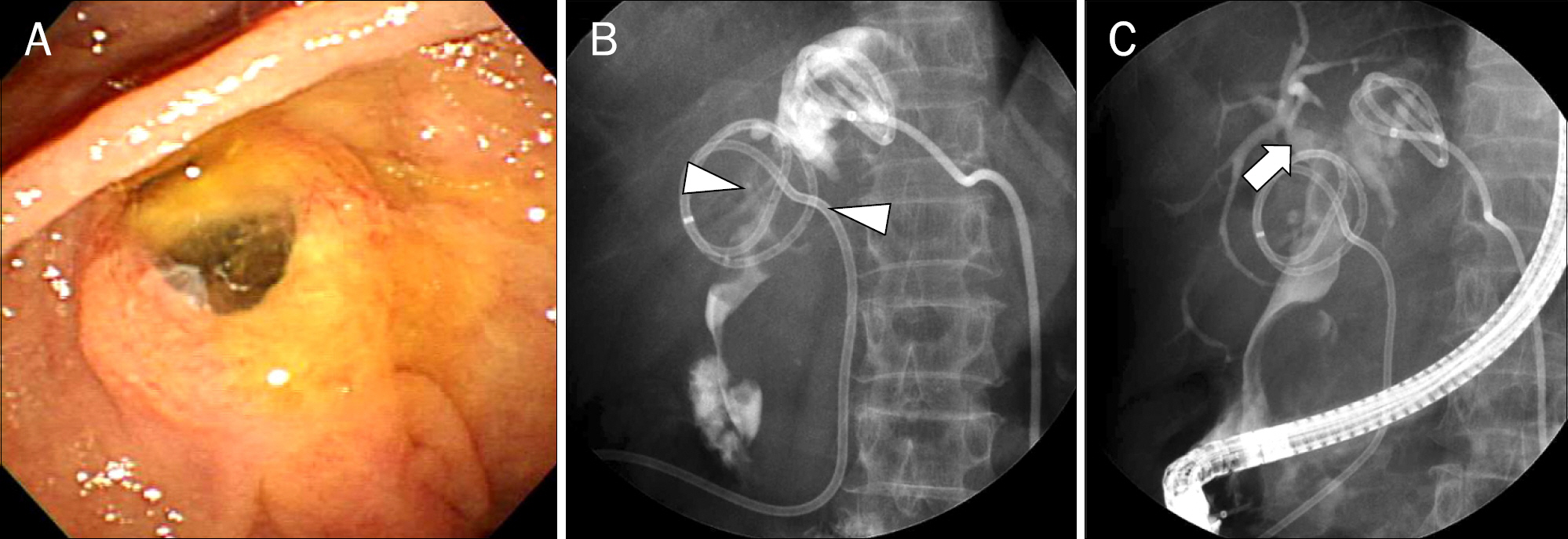
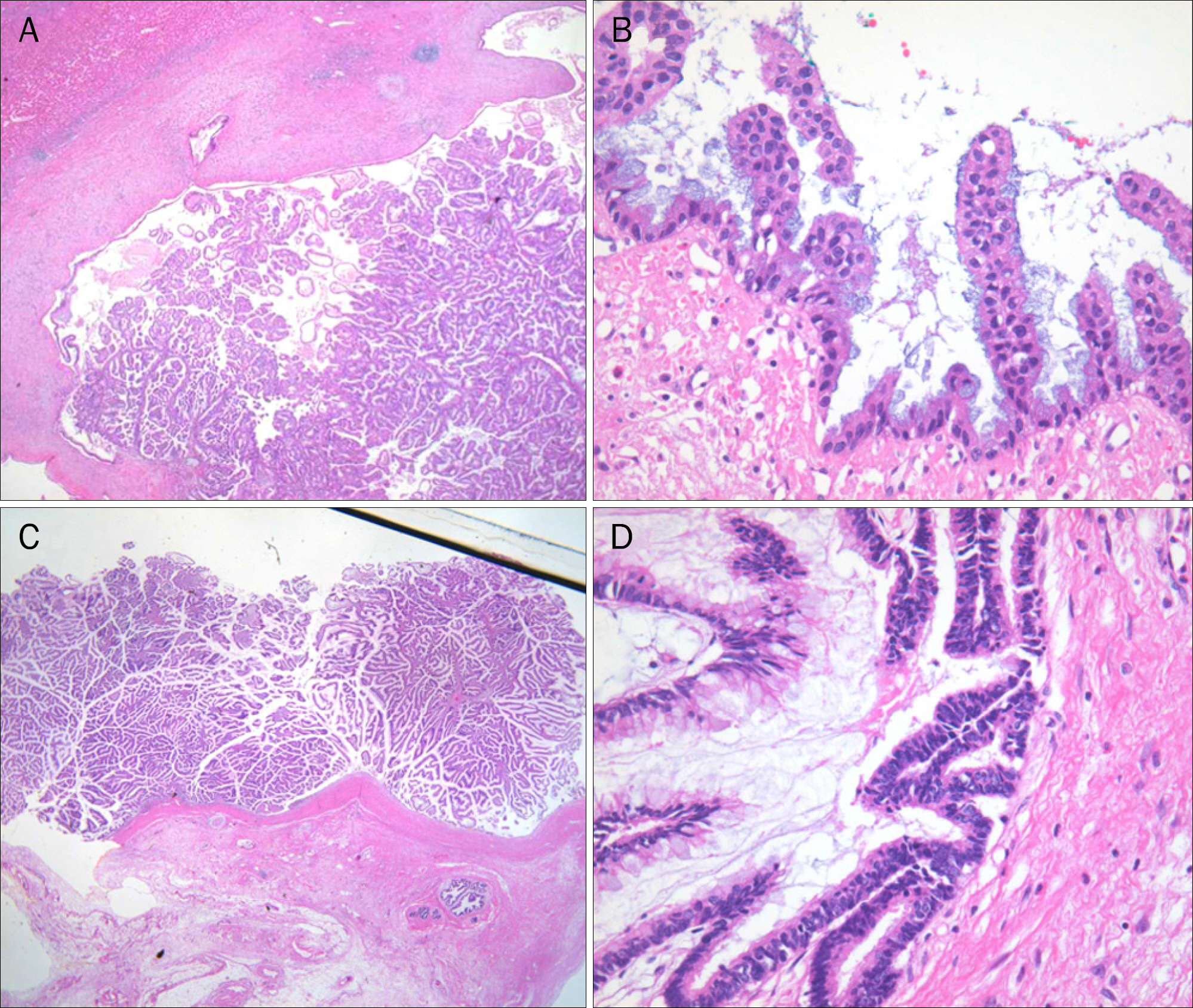
- Intraductal papillary mucinous neoplasm of the bile duct (IPMN-B) and intraductal papillary mucinous neoplasm of the pancreas (IPMN-P) have striking similarities and are recognized as counterparts. However, simultaneous occurrence of IPMN-B and IPMN-P is extremely rare. A 66 year-old female presented with recurrent epigastric pain and fever. During the past 9 years, she had three clinical episodes related to intrahepatic duct stones and IPMN-P in the pancreas head and was managed by medical treatment. Laboratory test results at admission revealed leukocytosis (12,600/mm3) and elevated CA 19-9 level (1,200 U/mL). Imaging study demonstrated liver abscess in the Couinaud's segment 4, IPMN-B in the left lobe, and IPMN-P in the whole pancreas with suspicious malignant change. Liver abscess was drained preoperatively, followed by left lobectomy with bile duct resection and total pancreatectomy with splenectomy. On histologic examination, non-invasive intraductal papillary mucinous carcinoma arising from various degree of dysplastic mucosa of the liver and pancreas could be observed. However, there was no continuity between the hepatic and pancreatic lesions. This finding in our case supports the theory that double primary lesions are more likely explained by a diffuse IPMN leading to synchronous tumors arising from both biliary and pancreatic ducts rather than by a metastatic process. Herein we present a case of simultaneous IPMN of the bile duct and pancreas which was successfully treated by surgical management.
MeSH Terms
-
Adenocarcinoma, Mucinous/*diagnosis/pathology/surgery
Adenocarcinoma, Papillary/*diagnosis/pathology/surgery
Aged
Bile Duct Neoplasms/*diagnosis/pathology/surgery
Bile Ducts, Intrahepatic/pathology
CA-19-9 Antigen/analysis
Carcinoma, Pancreatic Ductal/*diagnosis/pathology/surgery
Female
Hepatectomy
Humans
Leukocytosis/diagnosis
Pancreatectomy
Pancreatic Neoplasms/*diagnosis/pathology/surgery
Tomography, X-Ray Computed
CA-19-9 Antigen
Figure
Reference
-
References
1. Hamilton SR, Aaltonen LA. WHO classification of tumours. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press;2000.2. Nakanuma Y, Sasaki M, Ishikawa A, Tsui W, Chen TC, Huang SF. Biliary papillary neoplasm of the liver. Histol Histopathol. 2002; 17:851–861.3. Shibahara H, Tamada S, Goto M, et al. Pathologic features of mu-cin-producing bile duct tumors: two histopathologic categories as counterparts of pancreatic intraductal papillary-mucinous neoplasms. Am J Surg Pathol. 2004; 28:327–338.4. Yamaguchi Y, Abe N, Imase K, et al. A case of mucin hypersecreting intraductal papillary carcinomas occurring simultaneously in liver and pancreas. Gastrointest Endosc. 2005; 61:330–334.
Article5. Ohhashi K, Murakami Y, Maruyama M, Takekoshi T, Ohta H, Ohhashi I. Four cases of mucous secreting pancreatic cancer. Prog Dig Endosc. 1982; 20:348–351.6. Loftus EV Jr, Olivares-Pakzad BA, Batts KP, et al. Intraductal pap-illary-mucinous tumors of the pancreas: clinicopathologic features, outcome, and nomenclature. Members of the Pancreas Clinic, and Pancreatic Surgeons of Mayo Clinic. Gastroenterology. 1996; 110:1909–1918.
Article7. Kim HJ, Kim MH, Lee SK, et al. Mucin-hypersecreting bile duct tumor characterized by a striking homology with an intraductal papillary mucinous tumor (IPMT) of the pancreas. Endoscopy. 2000; 32:389–393.
Article8. Zen Y, Fujii T, Itatsu K, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006; 44:1333–1343.
Article9. Klöppel G, Kosmahl M. Is the intraductal papillary mucinous neoplasia of the biliary tract a counterpart of pancreatic papillary mucinous neoplasm? J Hepatol. 2006; 44:249–250.
Article10. Joo YH, Kim MH, Lee SK, et al. A case of mucin-hypersecreting intrahepatic bile duct tumor associated with pancreatic intraductal papillary mucinous tumor. Gastrointest Endosc. 2000; 52:409–412.
Article11. Ishida M, Seki K, Honda K, et al. Intraductal mucinous tumors occurring simultaneously in the liver and pancreas. J Gastroenterol. 2002; 37:1073–1078.
Article12. Zalinski S, Paradis V, Valla D, Belghiti J. Intraductal papillary mucinous tumors of both biliary and pancreatic ducts. J Hepatol. 2007; 46:978–979.
Article13. Sugiyama M, Atomi Y. Extrapancreatic neoplasms occur with unusual frequency in patients with intraductal papillary mucinous tumors of the pancreas. Am J Gastroenterol. 1999; 94:470–473.
Article14. Izawa T, Obara T, Tanno S, Mizukami Y, Yanagawa N, Kohgo Y. Clonality and field cancerization in intraductal papillary-mucinous tumors of the pancreas. Cancer. 2001; 92:1807–1817.
Article15. Sugiyama M, Atomi Y. Intraductal papillary mucinous tumors of the pancreas: imaging studies and treatment strategies. Ann Surg. 1998; 228:685–691.16. Chen TC, Nakanuma Y, Zen Y, et al. Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology. 2001; 34:651–658.
Article17. Suh KS, Roh HR, Koh YT, Lee KU, Park YH, Kim SW. Clinicopathologic features of the intraductal growth type of peripheral cholangiocarcinoma. Hepatology. 2000; 31:12–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Photodynamic Therapy Followed by Left Hepatectomy Used to Treat an Intraductal Papillary Mucinous Neoplasm of the Bile Duct
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report
- Synchronous Undifferentiated Carcinoma of Gallbladder in a Patient with Intrahepatic Intraductal Papillary Mucinous Neoplasia (b-IPMN)
- Cystic Neoplasms and Intraductal Papillary Mucinous Neoplasms of the Pancreas
- Comparison of Mucinous Cystic Tumor and Intraductal Papillary Mucinous Tumor