Clin Orthop Surg.
2011 Jun;3(2):157-159. 10.4055/cios.2011.3.2.157.
The Natural History of Pediatric Trigger Thumb: A Study with a Minimum of Five Years Follow-up
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea. ghbaek@snu.ac.kr
- KMID: 1719314
- DOI: http://doi.org/10.4055/cios.2011.3.2.157
Abstract
- BACKGROUND
Pediatric trigger thumb is due to deformed flexion of the interphalangeal joint. We previously reported that pediatric trigger thumb can spontaneously resolve in > 60% of patients at the median follow-up of 48 months. The purpose of this study was to determine whether there were any more cases of resolution with a follow-up of more than 5 years and whether any residual deformities remain, and so to confirm the natural history of pediatric trigger thumb.
METHODS
We prospectively followed 87 thumbs in 67 patients with pediatric trigger thumb and these patients didn't receive any treatment such as passive stretching, splinting or surgery. The date of the first visit ranged from April 1994 to March 2005. The patients were evaluated every six-months prior to resolution and annually after resolution. The median duration of follow-up was 87.3 months (range, 60 to 156 months).
RESULTS
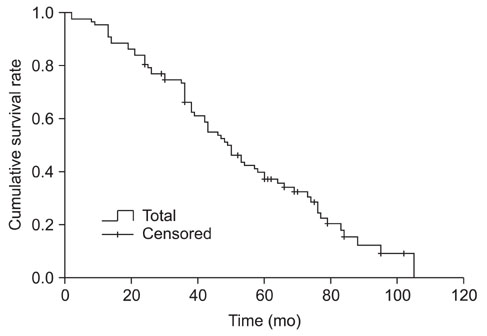
Of the 87 trigger thumbs, 66 (75.9%) resolved spontaneously. The median time from the initial visit to resolution was 49.0 months (95% confidence interval, 41.1 to 56.9). There were no residual deformities that resolved beyond 48 months. Although complete resolution did not occur in the remaining 21 thumbs, the flexion deformities did improve in all 21 thumbs. There were no other differences between the two groups besides the average duration of follow-up. There was no difference in resolution based on gender.
CONCLUSIONS
Pediatric trigger thumb can spontaneously resolve in > 75% of the cases after a follow-up period of at least 5 years. An operation may be delayed or avoided in the majority of cases. This may help both the families and the surgeons make decisions regarding the proper treatment of pediatric trigger thumb.
MeSH Terms
Figure
Reference
-
1. Baek GH, Kim JH, Chung MS, Kang SB, Lee YH, Gong HS. The natural history of pediatric trigger thumb. J Bone Joint Surg Am. 2008. 90(5):980–985.
Article2. Dinham JM, Meggitt BF. Trigger thumbs in children: a review of the natural history and indications for treatment in 105 patients. J Bone Joint Surg Br. 1974. 56(1):153–155.3. Michifuri Y, Murakami T, Kumagai S, Oyama M. Natural history of the trigger fingers in children. Seikei Geka. 1978. 29:1648–1651.4. Nemoto K, Nemoto T, Terada N, Amako M, Kawaguchi M. Splint therapy for trigger thumb and finger in children. J Hand Surg Br. 1996. 21(3):416–418.
Article5. Mulpruek P, Prichasuk S. Spontaneous recovery of trigger thumbs in children. J Hand Surg Br. 1998. 23(2):255–257.
Article6. Dunsmuir RA, Sherlock DA. The outcome of treatment of trigger thumb in children. J Bone Joint Surg Br. 2000. 82(5):736–738.
Article7. Moon WN, Suh SW, Kim IC. Trigger digits in children. J Hand Surg Br. 2001. 26(1):11–12.
Article8. Watanabe H, Hamada Y, Toshima T. Conservative management of infantile trigger thumb: indications and limitations. Tech Hand Up Extrem Surg. 2003. 7(1):37–42.
Article9. Tan AH, Lam KS, Lee EH. The treatment outcome of trigger thumb in children. J Pediatr Orthop B. 2002. 11(3):256–259.
Article10. Lee ZL, Chang CH, Yang WY, Hung SS, Shih CH. Extension splint for trigger thumb in children. J Pediatr Orthop. 2006. 26(6):785–787.
Article