Clin Orthop Surg.
2012 Dec;4(4):313-320. 10.4055/cios.2012.4.4.313.
Minimally Invasive Plate Osteosynthesis for Open Fractures of the Proximal Tibia
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyungpook National University Hospital, Daegu, Korea. cwoh@knu.ac.kr
- KMID: 1719300
- DOI: http://doi.org/10.4055/cios.2012.4.4.313
Abstract
- BACKGROUND
Relatively few studies have addressed plate osteosynthesis for open proximal tibial fractures by now. The purpose of this study was to assess the results of minimally invasive plate osteosynthesis (MIPO) for open fractures of the proximal tibia.
METHODS
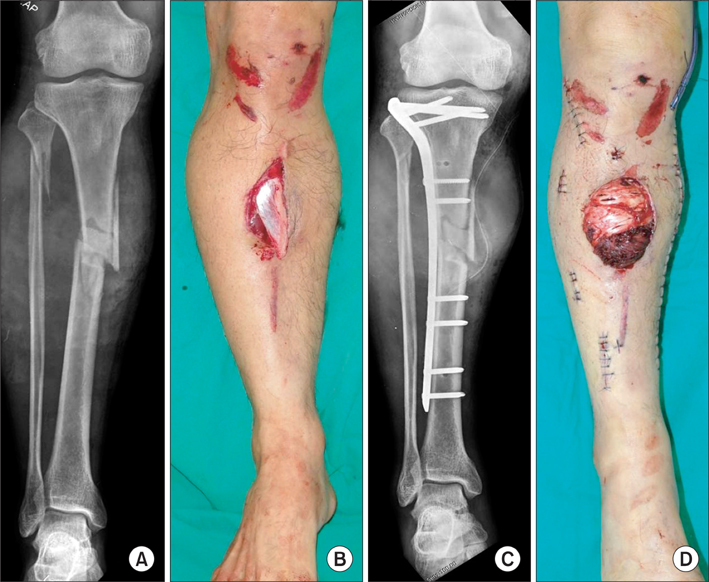
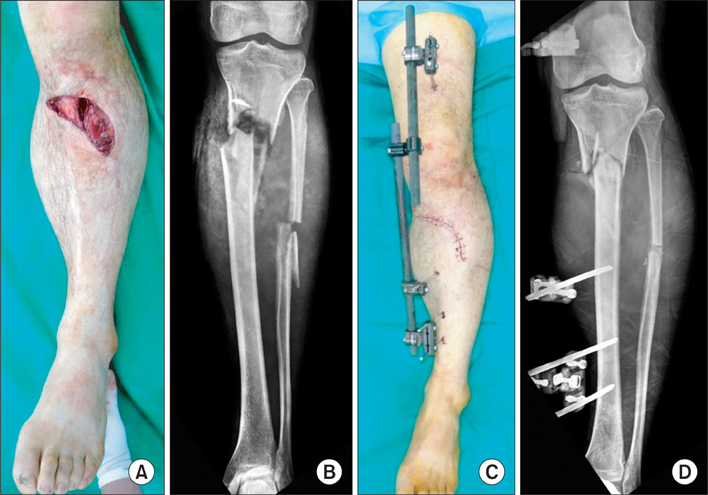
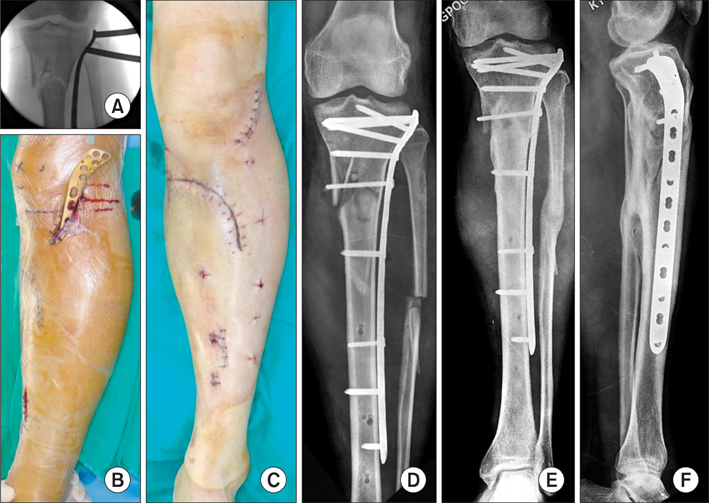
Thirty-four patients with an open proximal tibial fracture were treated by MIPO. Thirty of these, who followed for over 1 year, constituted the subject of this retrospective study. According to the AO Foundation and Orthopaedic Trauma Association (AO-OTA) classification, there were 3 patients of type 41-C, 6 of type 42-A, 8 of type 42-B, and 13 of type 42-C. In terms of the Gustilo and Anderson's open fracture grading system, 11 patients were of grade I, 6 were of grade II, and 13 were of grade III (III-A, 6; III-B, 6; III-C, 1). After thorough debridement and wound cleansing, when necessary, a soft tissue flap was placed. Primary MIPO (simultaneous plate fixation with soft tissue procedures) was performed in 18 patients, and staged MIPO (temporary external fixation followed by soft tissue procedures and subsequent conversion to plate fixation after soft tissue healing) was performed in 12 patients. Results were assessed according to the achievement and time to union, complications (including infections), and function of the knee joint using Knee Society scores. Statistical analysis was performed to identify factors influencing results.
RESULTS
Primary union was achieved by 24 of the 30 study subjects. Early bone grafting was performed in 6 cases with a massive initial bone defect expected to result in non-union. No patient had malalignment greater than 10degrees. The mean Knee Society score was 88.7 at final follow-up visits, 23 patients achieved an excellent result, and 7 a good result. There were 3 superficial and 5 deep infections, but none required early implant removal. Functional results were similar for primary and staged MIPO (p = 0.113). Fracture pattern (p = 0.089) and open fracture grade (p = 0.079) were not found to influence the results.
CONCLUSIONS
If soft tissue coverage is adequately performed, MIPO could be regarded as an acceptable method for the treatment of open proximal tibial fracture.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Outcomes of Severe Comminuted Distal Radius Fractures with Pronator Preserving Approach
Seung Hyun Cho, Hong Gi Park, Deuk Soo Jun, Jae Ang Sim, Young Hak Roh, Yong-Cheol Yoon, Jong-Ryoon Baek
J Korean Fract Soc. 2015;28(3):178-185. doi: 10.12671/jkfs.2015.28.3.178.
Reference
-
1. Starman JS, Castillo RC, Bosse MJ, MacKenzie EJ. LEAP Study Group. Proximal tibial metaphyseal fractures with severe soft tissue injury: clinical and functional results at 2 years. Clin Orthop Relat Res. 2010. 468(6):1669–1675.
Article2. Tejwani NC, Achan P. Staged management of high-energy proximal tibia fractures. Bull Hosp Jt Dis. 2004. 62(1-2):62–66.3. Clancey GJ, Hansen ST Jr. Open fractures of the tibia: a review of one hundred and two cases. J Bone Joint Surg Am. 1978. 60(1):118–122.4. Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994. 23(2):149–154.5. Whittle AP, Russell TA, Taylor JC, Lavelle DG. Treatment of open fractures of the tibial shaft with the use of interlocking nailing without reaming. J Bone Joint Surg Am. 1992. 74(8):1162–1171.
Article6. Kumar A, Whittle AP. Treatment of complex (Schatzker Type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma. 2000. 14(5):339–344.
Article7. Cole PA, Zlowodzki M, Kregor PJ. Less Invasive Stabilization System (LISS) for fractures of the proximal tibia: indications, surgical technique and preliminary results of the UMC Clinical Trial. Injury. 2003. 34:Suppl 1. A16–A29.
Article8. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000. (375):69–77.
Article9. Oh CW, Oh JK, Kyung HS, et al. Double plating of unstable proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. Acta Orthop. 2006. 77(3):524–530.
Article10. Oh JK, Oh CW, Jeon IH, et al. Percutaneous plate stabilization of proximal tibial fractures. J Trauma. 2005. 59(2):431–437.
Article11. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989. (248):13–14.
Article12. Das De S, Bae DS, Waters PM. Displaced humeral lateral condyle fractures in children: should we bury the pins? J Pediatr Orthop. 2012. 32(6):573–578.13. Bach AW, Hansen ST Jr. Plates versus external fixation in severe open tibial shaft fractures: a randomized trial. Clin Orthop Relat Res. 1989. (241):89–94.14. Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation of comminuted tibial plateau fractures. Clin Orthop Relat Res. 1996. (328):203–210.
Article15. Dendrinos GK, Kontos S, Katsenis D, Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996. 78(5):710–717.
Article16. Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma. 1998. 12(1):1–7.
Article17. Xue D, Zheng Q, Li H, Qian S, Zhang B, Pan Z. Reamed and unreamed intramedullary nailing for the treatment of open and closed tibial fractures: a subgroup analysis of randomised trials. Int Orthop. 2010. 34(8):1307–1313.
Article18. Lindvall E, Sanders R, Dipasquale T, Herscovici D, Haidukewych G, Sagi C. Intramedullary nailing versus percutaneous locked plating of extra-articular proximal tibial fractures: comparison of 56 cases. J Orthop Trauma. 2009. 23(7):485–492.
Article19. Nork SE, Barei DP, Schildhauer TA, et al. Intramedullary nailing of proximal quarter tibial fractures. J Orthop Trauma. 2006. 20(8):523–528.
Article20. Ricci WM, O'Boyle M, Borrelli J, Bellabarba C, Sanders R. Fractures of the proximal third of the tibial shaft treated with intramedullary nails and blocking screws. J Orthop Trauma. 2001. 15(4):264–270.
Article21. Stannard JP, Finkemeier CG, Lee J, Kregor PJ. Utilization of the less-invasive stabilization system internal fixator for open fractures of the proximal tibia: a multi-center evaluation. Indian J Orthop. 2008. 42(4):426–430.
Article22. Haidukewych GJ. Temporary external fixation for the management of complex intra- and periarticular fractures of the lower extremity. J Orthop Trauma. 2002. 16(9):678–685.
Article23. Ma CH, Wu CH, Yu SW, Yen CY, Tu YK. Staged external and internal less-invasive stabilisation system plating for open proximal tibial fractures. Injury. 2010. 41(2):190–196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Minimally Invasive Plate Osteosynthesis for Periarticular Tibial Fractures
- Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures