Korean J Radiol.
2013 Aug;14(4):576-580. 10.3348/kjr.2013.14.4.576.
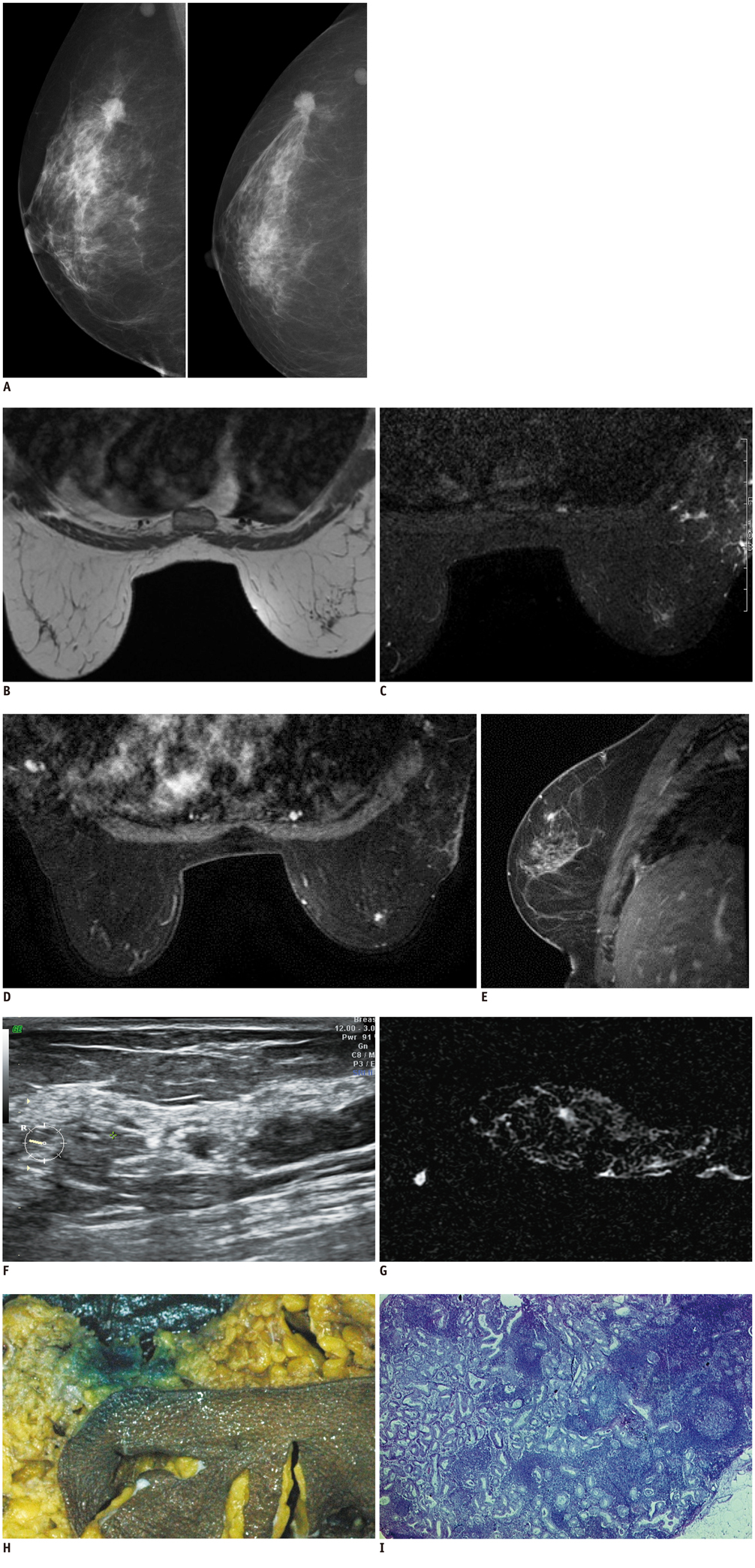
Diagnosis of a Malignant Intramammary Node Retrospectively Aided by Mastectomy Specimen MRI-Is the Search Worth It? A Case Report and Review of Current Literature
- Affiliations
-
- 1Department of Radiodiagnosis, Tata Memorial Hospital, Mumbai 400012, India. amarudare@gmail.com
- 2Department of Pathology, Tata Memorial Hospital, Mumbai 400012, India.
- KMID: 1715761
- DOI: http://doi.org/10.3348/kjr.2013.14.4.576
Abstract
- Metastases to intramammary nodes have been shown to be an independent predictor of poor outcome in patients with breast cancer, such as axillary lymph node metastases. The detection and accurate characterization of these nodes preoperatively is thus crucial for the staging and planning of treatment for breast carcinoma, particularly in cases with axillary lymph node negative disease as it upgrades the disease staging. We herein report the first case where we detected an intra-mammary node on specimen MRI after the primary pathological gross specimen evaluation failed to detect the node.
MeSH Terms
Figure
Reference
-
1. Hogan BV, Peter MB, Shenoy H, Horgan K, Shaaban A. Intramammary lymph node metastasis predicts poorer survival in breast cancer patients. Surg Oncol. 2010; 19:11–16.2. Stomper PC, Leibowich S, Meyer JE. The prevalence and distribution of well circumscribed nodules on screening mammography: analysis of 1500 mammograms. Breast Dis. 1991; 4:197–203.3. Svane G, Franzén S. Radiologic appearance of nonpalpable intramammary lymph nodes. Acta Radiol. 1993; 34:577–580.4. Egan RL. Breast imaging: diagnosis and morphology of breast diseases. Philadelphia, Pa: Saunders;1988. p. 313–323.5. Lindfors KK, Kopans DB, Googe PB, McCarthy KA, Koerner FC, Meyer JE. Breast cancer metastasis to intramammary lymph nodes. AJR Am J Roentgenol. 1986; 146:133–136.6. Lee CH, Giurescu ME, Philpotts LE, Horvath LJ, Tocino I. Clinical importance of unilaterally enlarging lymph nodes on otherwise normal mammograms. Radiology. 1997; 203:329–334.7. Shen J, Hunt KK, Mirza NQ, Krishnamurthy S, Singletary SE, Kuerer HM, et al. Intramammary lymph node metastases are an independent predictor of poor outcome in patients with breast carcinoma. Cancer. 2004; 101:1330–1337.8. Diaz R, Degnim AC, Boughey JC, Nassar A, Jakub JW. A positive intramammary lymph node does not mandate a complete axillary node dissection. Am J Surg. 2012; 203:151–155.9. McSweeney MB, Egan RL. Prognosis of breast cancer related to intramammary lymph nodes. Recent Results Cancer Res. 1984; 90:166–172.10. Guth AA, Mercado C, Roses DF, Hiotis K, Skinner K, Diflo T, et al. Intramammary lymph nodes and breast cancer: a marker for disease severity, or just another lymph node? Am J Surg. 2006; 192:502–505.11. Singletary SE, Connolly JL. Breast cancer staging: working with the sixth edition of the AJCC Cancer Staging Manual. CA Cancer J Clin. 2006; 56:37–47. quiz 50-51.12. Nassar A, Cohen C, Cotsonis G, Carlson G. Significance of intramammary lymph nodes in the staging of breast cancer: correlation with tumor characteristics and outcome. Breast J. 2008; 14:147–152.13. Pugliese MS, Stempel MM, Cody HS 3rd, Morrow M, Gemignani ML. Surgical management of the axilla: do intramammary nodes matter? Am J Surg. 2009; 198:532–537.14. Intra M, Garcia-Etienne CA, Renne G, Trifirò G, Rotmensz N, Gentilini OD, et al. When sentinel lymph node is intramammary. Ann Surg Oncol. 2008; 15:1304–1308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramammary sentinel lymph node with capsular extravasation in breast cancer
- Cavernous Hemangioma of Lymph node: A case report with the review of literature
- Invasive Paget’s Disease of the Breast: A case Report
- A case of malignant peripheral nerve sheath tumor of pelvic cavity
- Necrotic Complications in Nipple-Sparing Mastectomy Followed by Immediate Breast Reconstruction: Systematic Review with Pooled Analysis