Korean J Radiol.
2014 Apr;15(2):277-285. 10.3348/kjr.2014.15.2.277.
Impaired Coronary Flow Reserve Is the Most Important Marker of Viable Myocardium in the Myocardial Segment-Based Analysis of Dual-Isotope Gated Myocardial Perfusion Single-Photon Emission Computed Tomography
- Affiliations
-
- 1Department of Nuclear Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam 463-707, Korea.
- 2Institute of Radiation Medicine, Medical Research Center, Seoul National University, Seoul 110-744, Korea. dsl@plaza.snu.ac.kr
- 3Department of Nuclear Medicine, Konkuk University School of Medicine, Seoul 143-729, Korea.
- 4Department of Thoracic & Cardiovascular Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 110-744, Korea.
- 5Department of Nuclear Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 110-744, Korea.
- KMID: 1705584
- DOI: http://doi.org/10.3348/kjr.2014.15.2.277
Abstract
OBJECTIVE
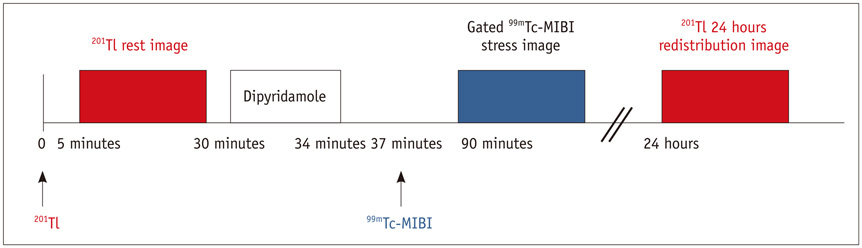
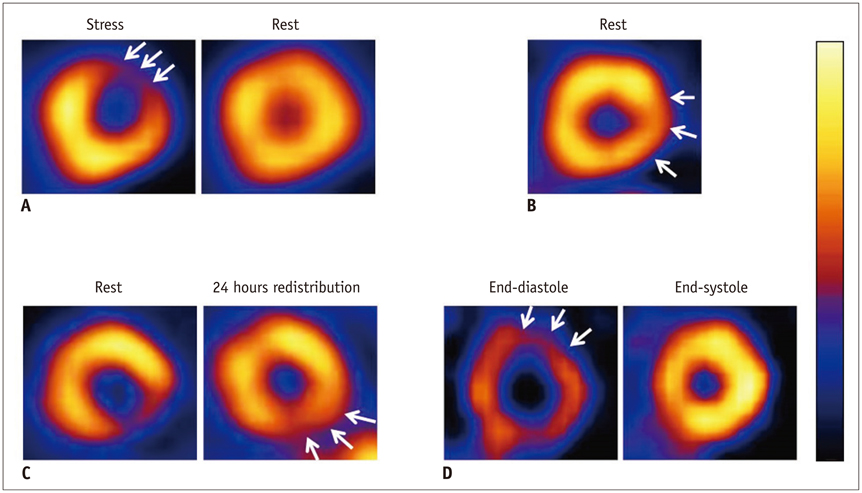
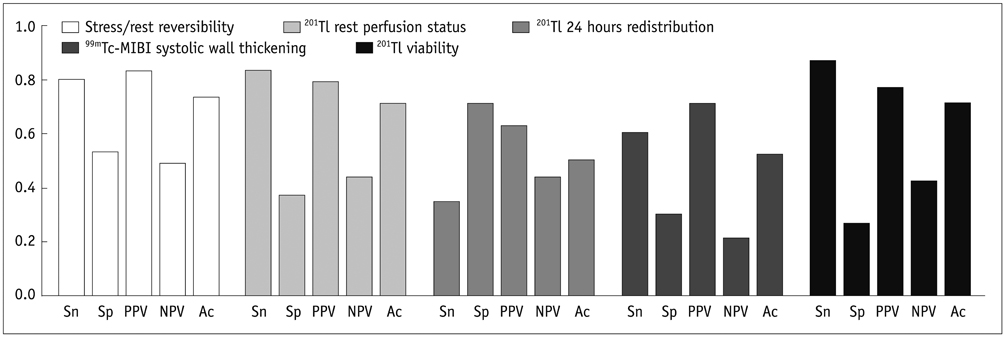
The aim of this study was to investigate the most robust predictor of myocardial viability among stress/rest reversibility (coronary flow reserve [CFR] impairment), 201Tl perfusion status at rest, 201Tl 24 hours redistribution and systolic wall thickening of 99mTc-methoxyisobutylisonitrile using a dual isotope gated myocardial perfusion single-photon emission computed tomography (SPECT) in patients with coronary artery disease (CAD) who were re-vascularized with a coronary artery bypass graft (CABG) surgery.
MATERIALS AND METHODS
A total of 39 patients with CAD was enrolled (34 men and 5 women), aged between 36 and 72 years (mean 58 +/- 8 standard in years) who underwent both pre- and 3 months post-CABG myocardial SPECT. We analyzed 17 myocardial segments per patient. Perfusion status and wall motion were semi-quantitatively evaluated using a 4-point grading system. Viable myocardium was defined as dysfunctional myocardium which showed wall motion improvement after CABG.
RESULTS
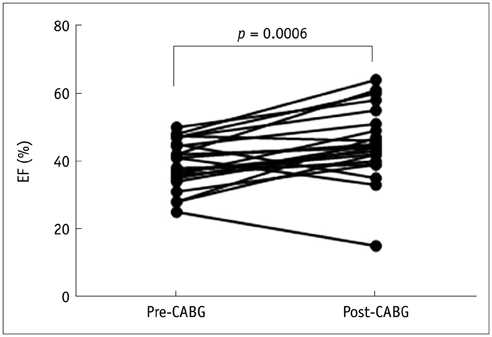
The left ventricular ejection fraction (LVEF) significantly increased from 37.8 +/- 9.0% to 45.5 +/- 12.3% (p < 0.001) in 22 patients who had a pre-CABG LVEF lower than 50%. Among 590 myocardial segments in the re-vascularized area, 115 showed abnormal wall motion before CABG and 73.9% (85 of 115) had wall motion improvement after CABG. In the univariate analysis (n = 115 segments), stress/rest reversibility (p < 0.001) and 201Tl rest perfusion status (p = 0.024) were significant predictors of wall motion improvement. However, in multiple logistic regression analysis, stress/rest reversibility alone was a significant predictor for post-CABG wall motion improvement (p < 0.001).
CONCLUSION
Stress/rest reversibility (impaired CFR) during dual-isotope gated myocardial perfusion SPECT was the single most important predictor of wall motion improvement after CABG.
Keyword
MeSH Terms
-
Adult
Aged
Analysis of Variance
Cardiac-Gated Single-Photon Emission Computer-Assisted Tomography/*methods
Coronary Artery Bypass
Coronary Artery Disease/physiopathology/*radionuclide imaging/surgery
Coronary Circulation/*physiology
Coronary Disease/radionuclide imaging/surgery
Female
Humans
Male
Middle Aged
Myocardial Contraction/physiology
Myocardium
Nitriles/diagnostic use
Stroke Volume/physiology
Technetium/diagnostic use
Ventricular Function, Left/physiology
Nitriles
Technetium
Figure
Reference
-
1. Rahimtoola SH. Coronary bypass surgery for chronic angina--1981. A perspective. Circulation. 1982; 65:225–241.2. Iskandrian AS. Myocardial viability: unresolved issues. J Nucl Med. 1996; 37:794–797.3. Ragosta M, Beller GA, Watson DD, Kaul S, Gimple LW. Quantitative planar rest-redistribution 201Tl imaging in detection of myocardial viability and prediction of improvement in left ventricular function after coronary bypass surgery in patients with severely depressed left ventricular function. Circulation. 1993; 87:1630–1641.4. Taki J, Nakajima K, Bunko H, Kawasuji M, Tonami N, Hisada K. Twenty-four-hour quantitative thallium imaging for predicting beneficial revascularization. Eur J Nucl Med. 1994; 21:1212–1217.5. Zimmermann R, Mall G, Rauch B, Zimmer G, Gabel M, Zehelein J, et al. Residual 201Tl activity in irreversible defects as a marker of myocardial viability. Clinicopathological study. Circulation. 1995; 91:1016–1021.6. Dilsizian V, Rocco TP, Freedman NM, Leon MB, Bonow RO. Enhanced detection of ischemic but viable myocardium by the reinjection of thallium after stress-redistribution imaging. N Engl J Med. 1990; 323:141–146.7. Ohtani H, Tamaki N, Yonekura Y, Mohiuddin IH, Hirata K, Ban T, et al. Value of thallium-201 reinjection after delayed SPECT imaging for predicting reversible ischemia after coronary artery bypass grafting. Am J Cardiol. 1990; 66:394–399.8. Snapper HJ, Shea NL, Konstam MA, Oates E, Udelson JE. Combined analysis of resting regional wall thickening and stress perfusion with electrocardiographic-gated technetium 99m-labeled sestamibi single-photon emission computed tomography: prediction of stress defect reversibility. J Nucl Cardiol. 1997; 4(1 Pt 1):3–10.9. Berman DS, Kiat H, Friedman JD, Wang FP, van Train K, Matzer L, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual-isotope myocardial perfusion single-photon emission computed tomography: a clinical validation study. J Am Coll Cardiol. 1993; 22:1455–1464.10. Chua T, Kiat H, Germano G, Maurer G, van Train K, Friedman J, et al. Gated technetium-99m sestamibi for simultaneous assessment of stress myocardial perfusion, postexercise regional ventricular function and myocardial viability. Correlation with echocardiography and rest thallium-201 scintigraphy. J Am Coll Cardiol. 1994; 23:1107–1114.11. Cho SG, Kim JH, Cho JY, Kim HS, Bom HS. Myocardial blood flow and flow reserve in proximal and mid-to-distal lesions of left anterior descending artery measured by N-13 ammonia PET/CT. Nucl Med Mol Imaging. 2013; 47:158–165.12. Matzer L, Kiat H, Wang FP, Van Train K, Germano G, Friedman J, et al. Pharmacologic stress dual-isotope myocardial perfusion single-photon emission computed tomography. Am Heart J. 1994; 128(6 Pt 1):1067–1076.13. Mazzanti M, Germano G, Kiat H, Kavanagh PB, Alexanderson E, Friedman JD, et al. Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol. 1996; 27:1612–1620.14. Hachamovitch R, Kang X, Amanullah AM, Abidov A, Hayes SW, Friedman JD, et al. Prognostic implications of myocardial perfusion single-photon emission computed tomography in the elderly. Circulation. 2009; 120:2197–2206.15. Rozanski A, Berman DS, Gray R, Levy R, Raymond M, Maddahi J, et al. Use of thallium-201 redistribution scintigraphy in the preoperative differentiation of reversible and nonreversible myocardial asynergy. Circulation. 1981; 64:936–944.16. Alfieri O, La Canna G, Giubbini R, Pardini A, Zogno M, Fucci C. Recovery of myocardial function. The ultimate target of coronary revascularization. Eur J Cardiothorac Surg. 1993; 7:325–330. discussion 330.17. Bonow RO, Maurer G, Lee KL, Holly TA, Binkley PF, Desvigne-Nickens P, et al. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011; 364:1617–1625.18. Fallavollita JA, Canty JM Jr. Differential 18F-2-deoxyglucose uptake in viable dysfunctional myocardium with normal resting perfusion: evidence for chronic stunning in pigs. Circulation. 1999; 99:2798–2805.19. Shah BN, Khattar RS, Senior R. The hibernating myocardium: current concepts, diagnostic dilemmas, and clinical challenges in the post-STICH era. Eur Heart J. 2013; 34:1323–1336.20. Lim H, Fallavollita JA, Hard R, Kerr CW, Canty JM Jr. Profound apoptosis-mediated regional myocyte loss and compensatory hypertrophy in pigs with hibernating myocardium. Circulation. 1999; 100:2380–2386.21. Margonato A, Mailhac A, Bonetti F, Vicedomini G, Fragasso G, Landoni C, et al. Exercise-induced ischemic arrhythmias in patients with previous myocardial infarction: role of perfusion and tissue viability. J Am Coll Cardiol. 1996; 27:593–598.22. Afridi I, Kleiman NS, Raizner AE, Zoghbi WA. Dobutamine echocardiography in myocardial hibernation. Optimal dose and accuracy in predicting recovery of ventricular function after coronary angioplasty. Circulation. 1995; 91:663–670.23. Paeng JC, Lee DS, Kang WJ, Lee BI, Kim KB, Chung JK, et al. Time course of functional recovery after coronary artery bypass grafting surgery according to the preoperative reversibility of perfusion impairment on myocardial SPECT. Eur J Nucl Med Mol Imaging. 2005; 32:70–74.24. Smart SC. The clinical utility of echocardiography in the assessment of myocardial viability. J Nucl Med. 1994; 35:4 Suppl. 49S–58S.25. Lee WW, Park EK, Eo JS, Lee SW, Kim CH, So Y, et al. Evaluation of immediate post-stress wall motion on adenosine stress/rest thallium-201 gated myocardial SPECT. Int J Cardiovasc Imaging. 2006; 22:213–222.26. Beanlands RS, Nichol G, Huszti E, Humen D, Racine N, Freeman M, et al. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2). J Am Coll Cardiol. 2007; 50:2002–2012.27. Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011; 364:1607–1616.28. Schinkel AF, Poldermans D, Elhendy A, Bax JJ. Assessment of myocardial viability in patients with heart failure. J Nucl Med. 2007; 48:1135–1146.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantitative gated myocardial perfusion SPECT
- Quantification of Myocardial Perfusion and Function Using SPECT and PET
- Assessment of Viable Myocardium with Nuclear Imaging
- Correlation Between Functional Myocardial Perfusion Imaging and Anatomical Cardiac CT in a Case of Myocardial Bridging
- Prognostic Value of Rest Tl-201/Dipyridamole Stress Tc-99m-MIBI Myocardial Single Photon Emission Computed Tomography (SPECT)