Non-Ischemic Perfusion Defects due to Delayed Arrival of Contrast Material on Stress Perfusion Cardiac Magnetic Resonance Imaging after Coronary Artery Bypass Graft Surgery
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul 110-744, Korea. iameuna1@gmail.com
- 2Department of Neuclear Medicine, Seoul National University Hospital, Seoul 110-744, Korea.
- KMID: 1705572
- DOI: http://doi.org/10.3348/kjr.2014.15.2.188
Abstract
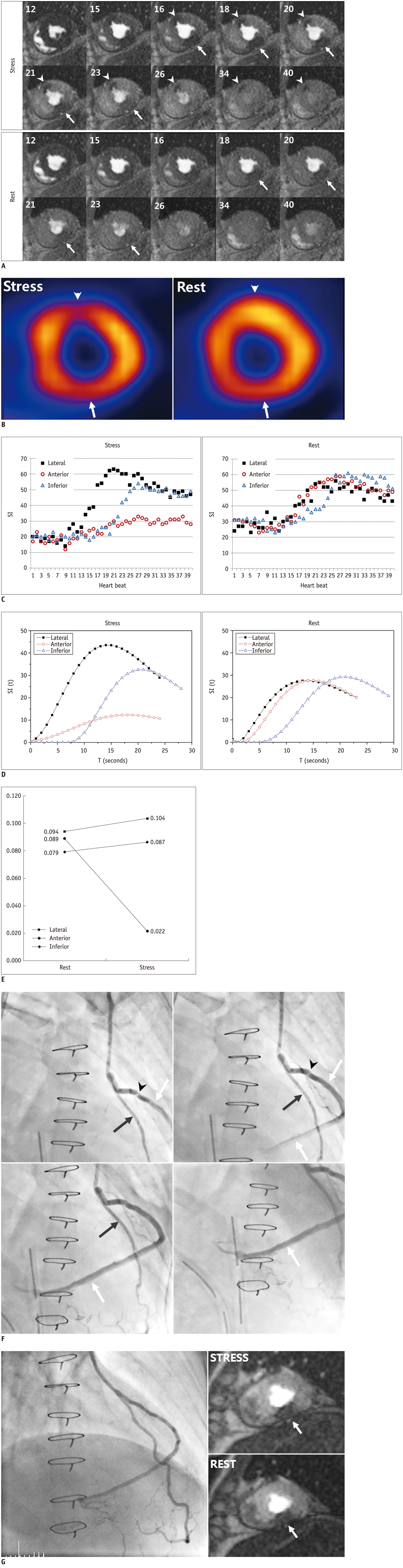
- Herein we report about the adenosine stress perfusion MR imaging findings of a 50-year-old man who exhibited two different perfusion defects resulting from two different mechanisms after a coronary artery bypass surgery. An invasive coronary angiography confirmed that one perfusion defect at the mid-anterior wall resulted from an ischemia due to graft stenosis. However, no stenosis was detected on the graft responsible for the mid-inferior wall showing the other perfusion defect. It was assumed that the perfusion defect at the mid-inferior wall resulted from delayed perfusion owing to the long pathway of the bypass graft. The semiquantitative analysis of corrected signal-time curves supported our speculation, demonstrating that the rest-to-stress ratio index of the maximal slope of the myocardial territory in question was similar to those of normal myocardium, whereas that of myocardium with the stenotic graft showed a typical ischemic pattern. A delayed perfusion during long graft pathway in a post-bypass graft patient can mimick a true perfusion defect on myocardial stress MR imaging. Radiologists should be aware of this knowledge to avoid misinterpretation of graft and myocardial status in post bypass surgery patients.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging—Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, JeongJae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae Young Lee
Korean J Radiol. 2019;20(12):1562-1582. doi: 10.3348/kjr.2019.0411.Guidelines for Cardiovascular Magnetic Resonance Imaging from the Korean Society of Cardiovascular Imaging (KOSCI) - Part 3: Perfusion, Delayed Enhancement, and T1- and T2 Mapping
Dong Jin Im, Su Jin Hong, Eun-Ah Park, Eun Young Kim, Yeseul Jo, Jeong Jae Kim, Chul Hwan Park, Hwan Seok Yong, Jae Wook Lee, Jee Hye Hur, Dong Hyun Yang, Bae-Young Lee
Investig Magn Reson Imaging. 2020;24(1):1-20. doi: 10.13104/imri.2020.24.1.1.
Reference
-
1. Schwitter J, Nanz D, Kneifel S, Bertschinger K, Büchi M, Knüsel PR, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation. 2001; 103:2230–2235.2. Ibrahim T, Nekolla SG, Schreiber K, Odaka K, Volz S, Mehilli J, et al. Assessment of coronary flow reserve: comparison between contrast-enhanced magnetic resonance imaging and positron emission tomography. J Am Coll Cardiol. 2002; 39:864–870.3. Nagel E, Klein C, Paetsch I, Hettwer S, Schnackenburg B, Wegscheider K, et al. Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation. 2003; 108:432–437.4. Su MY, Yang KC, Wu CC, Wu YW, Yu HY, Tseng RY, et al. First-pass myocardial perfusion cardiovascular magnetic resonance at 3 Tesla. J Cardiovasc Magn Reson. 2007; 9:633–644.5. Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol. 2003; 41:159–168.6. Bernhardt P, Spiess J, Levenson B, Pilz G, Höfling B, Hombach V, et al. Combined assessment of myocardial perfusion and late gadolinium enhancement in patients after percutaneous coronary intervention or bypass grafts: a multicenter study of an integrated cardiovascular magnetic resonance protocol. JACC Cardiovasc Imaging. 2009; 2:1292–1300.7. Klein C, Nagel E, Gebker R, Kelle S, Schnackenburg B, Graf K, et al. Magnetic resonance adenosine perfusion imaging in patients after coronary artery bypass graft surgery. JACC Cardiovasc Imaging. 2009; 2:437–445.8. al-Saadi N, Gross M, Bornstedt A, Schnackenburg B, Klein C, Fleck E, et al. [Comparison of various parameters for determining an index of myocardial perfusion reserve in detecting coronary stenosis with cardiovascular magnetic resonance tomography]. Z Kardiol. 2001; 90:824–834.9. Kelle S, Graf K, Dreysse S, Schnackenburg B, Fleck E, Klein C. Evaluation of contrast wash-in and peak enhancement in adenosine first pass perfusion CMR in patients post bypass surgery. J Cardiovasc Magn Reson. 2010; 12:28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Result of Coronary Artery Bypass Graft Surgery by Using Pre and Postoperative Myocardial SPECT
- Stress Testing and Imaging Protocols for Myocardial Perfusion Studies
- Myocardial Contractility, Perfusion, and Viability Analysis Using Multidetector CT in Patients with Ischemic Heart Disease
- MR Imaging of Ischemic Heart Disease
- Segmental Analysis of Thallium-201 Stress Myocardial Perfusion Scanning in Coronary Artery Disease