Clin Orthop Surg.
2013 Sep;5(3):195-201. 10.4055/cios.2013.5.3.195.
Usefulness of Prone Cross-Table Lateral Radiographs in Vertebral Compression Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea. bschang@snu.ac.kr
- 2Department of Orthopedic Surgery, Seoul National University Boramae Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1705545
- DOI: http://doi.org/10.4055/cios.2013.5.3.195
Abstract
- BACKGROUND
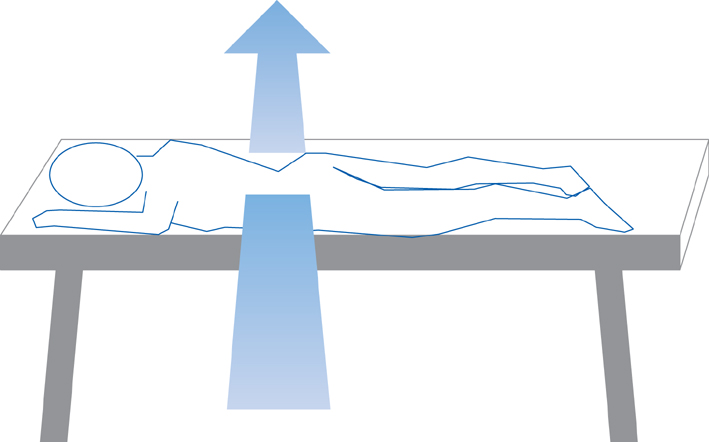
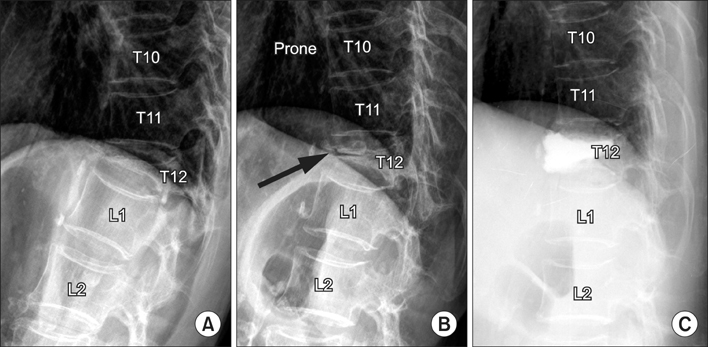
Dynamic radiographs are recommended to investigate non-healing evidence such as the dynamic mobility or intravertebral clefts in osteoporotic vertebral compression fractures (VCFs). However, it is difficult to examine standing flexion and extension lateral radiographs due to severe pain. The use of prone cross-table lateral radiographs (PrLRs) as a diagnostic tool has never been proposed to our knowledge. The purpose of this study is to clarify the usefulness of PrLRs in diagnosis and treatment of VCFs.
METHODS
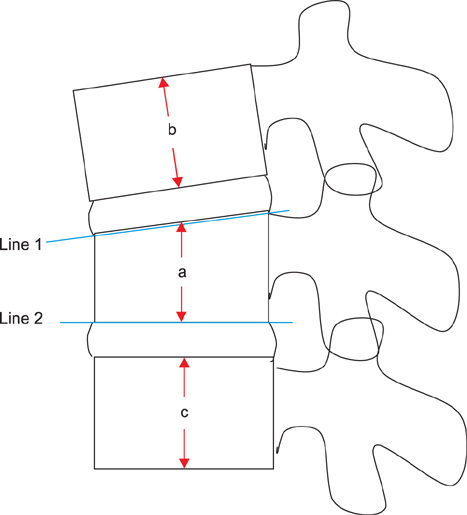
We reviewed 62 VCF patients examined with PrLRs between January 1, 2008 and June 30, 2011. To compare the degree of pain provoked between standing extension lateral radiographs (StLRs) and PrLRs, numeric rating scale (NRS) scores were assessed and compared by a paired t-test. Vertebroplasty was done for 40 patients and kyphoplasty was done for 9 patients with routine manners. To assess the degree of postural reduction, vertebral wedge angles (VWA) and vertebral height ratios (VHR) were calculated by using preoperative StLRs, PrLRs, and postoperative lateral radiographs. Two variables derived from changes in VWA and VHR between preoperative and postoperative radiographs were compared by a paired t-test.
RESULTS
The average NRS scores were 6.23 +/- 1.67 in StLRs and 5.18 +/- 1.47 in PrLRs. The degree of pain provocation was lower in using PrLRs than StLRs (p < 0.001). The average changes of VWA between preoperative and postoperative status were 5.24degrees +/- 6.16degrees with PrLRs and 3.46degrees +/- 3.47degrees with StLRs. The average changes of VHR were 0.248 +/- 0.178 with PrLRs and 0.148 +/- 0.161 with StLRs. The comparisons by two variables showed significant differences for both parameters (p = 0.021 and p < 0.001, respectively). The postoperative radiological status was reflected more precisely when using PrLRs than StLRs.
CONCLUSIONS
In comparison with StLR, the PrLR was more accurate in predicting the degree of restoration of postoperative vertebral heights and wedge angles, and provoked less pain during examination. The PrLR could be a useful diagnostic tool to detect intravertebral cleft or intravertebral dynamic instability.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Posttraumatic Delayed Vertebral Collapse : Kummell’s Disease
Jeongwook Lim, Seung-Won Choi, Jin-Young Youm, Hyon-Jo Kwon, Seon-Hwan Kim, Hyeon-Song Koh
J Korean Neurosurg Soc. 2018;61(1):1-9. doi: 10.3340/jkns.2017.0505.010.
Reference
-
1. Klazen CA, Verhaar HJ, Lohle PN, et al. Clinical course of pain in acute osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2010; 21(9):1405–1409.
Article2. Freedman BA, Heller JG. Kummel disease: a not-so-rare complication of osteoporotic vertebral compression fractures. J Am Board Fam Med. 2009; 22(1):75–78.
Article3. McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum. 2003; 48(5):1414–1419.
Article4. McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 2003; 18(1):24–29.
Article5. Wu MH, Huang TJ, Cheng CC, Li YY, Hsu RW. Role of the supine lateral radiograph of the spine in vertebroplasty for osteoporotic vertebral compression fracture: a prospective study. BMC Musculoskelet Disord. 2010; 11:164.
Article6. Chen YJ, Lo DF, Chang CH, Chen HT, Hsu HC. The value of dynamic radiographs in diagnosing painful vertebrae in osteoporotic compression fractures. AJNR Am J Neuroradiol. 2011; 32(1):121–124.
Article7. Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J. 2004; 4(4):418–424.
Article8. Erkan S, Ozalp TR, Yercan HS, Okcu G. Does timing matter in performing kyphoplasty? Acute versus chronic compression fractures. Acta Orthop Belg. 2009; 75(3):396–404.9. McKiernan F, Faciszewski T, Jensen R. Reporting height restoration in vertebral compression fractures. Spine (Phila Pa 1976). 2003; 28(22):2517–2521.
Article10. Gangi A, Sabharwal T, Irani FG, et al. Quality assurance guidelines for percutaneous vertebroplasty. Cardiovasc Intervent Radiol. 2006; 29(2):173–178.
Article11. Eck JC, Nachtigall D, Humphreys SC, Hodges SD. Comparison of vertebroplasty and balloon kyphoplasty for treatment of vertebral compression fractures: a meta-analysis of the literature. Spine J. 2008; 8(3):488–497.
Article12. Li X, Yang H, Tang T, Qian Z, Chen L, Zhang Z. Comparison of kyphoplasty and vertebroplasty for treatment of painful osteoporotic vertebral compression fractures: twelve-month follow-up in a prospective nonrandomized comparative study. J Spinal Disord Tech. 2012; 25(3):142–149.
Article13. Mathis JM, Ortiz AO, Zoarski GH. Vertebroplasty versus kyphoplasty: a comparison and contrast. AJNR Am J Neuroradiol. 2004; 25(5):840–845.
Article14. Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007; 7(5):575–582.
Article15. Brown DB, Gilula LA, Sehgal M, Shimony JS. Treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol. 2004; 182(2):319–322.
Article16. Tseng YY, Yang TC, Tu PH, Lo YL, Yang ST. Repeated and multiple new vertebral compression fractures after percutaneous transpedicular vertebroplasty. Spine (Phila Pa 1976). 2009; 34(18):1917–1922.
Article17. Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010; 19(11):1907–1912.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Factors that Affect the Deformity Correction of Vertebral Body during Kyphoplasty of Osteoporotic Vertebral Compression Fracture
- Radiographic Comparison of Stable Burst Fractures with Compression Fractures in Thoracolumbar Spine
- Spontaneous Height Restoration of Vertebral Compression Fracture: A Case Report
- Vertebral compression fractures: distinction between benign and malignant causes with Tc-99m labeled antigranulocyte antibody immunoscintigraphy
- One-stage multi-level vertebroplasty for a patient with a rapidly deteriorating condition due to multiple vertebral compression fractures: A case report