Tuberc Respir Dis.
2006 Jun;60(6):625-630. 10.4046/trd.2006.60.6.625.
Alteration of Coagulation and Fibrinolysis System According to Right Ventricular Dysfunction in Chronic Obstructive Pulmonary Disease
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. khj@yumc.yonsei.ac.kr
- 2Department of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea.
- KMID: 1630800
- DOI: http://doi.org/10.4046/trd.2006.60.6.625
Abstract
-
BACKGROUND: Pulmonary hypertension in COPD patients is the result of a direct effect of tobacco smoke on the intrapulmonary vessels with the abnormal production of the mediators that control vasoconstriction, vasodilatation, and vascular cell proliferation, which ultimately lead to aberrant vascular remodeling and physiology. COPD patients are prone to the developmint of an acute and chronic thromboembolism with an elevation of the plasma procoagulant and fibrinolytic markers However, the roles of the coagulation and fibrinolysis system on the right ventricular dysfunction in COPD patients are not well defined. We examined the alteration of the coagulation and fibrinolysis system in COPD patients according to the right ventricular function measured using cardiac multidetector computed tomography (MDCT).
METHODS
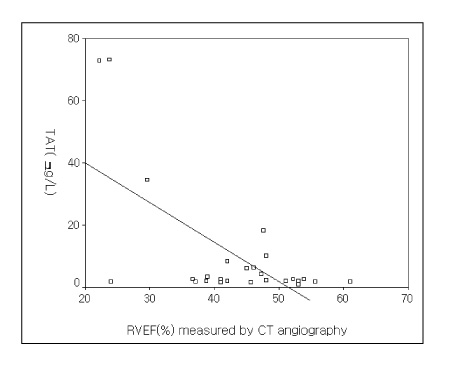
The right ventricular ejection fraction (RVEF) was measured using cardiac MDCT in 26 patients who were diagnosed with COPD according to the definition of the GOLD guideline. The plasma level of thrombin antithrombin (TAT) and plasminogen activator inhibitor (PAI)-1 were measured using an enzyme linked immunoassay.
RESULTS
The plasma TAT was markedly elevated in COPD patients (10.5+/-19.8microgram/L) compared with those of the control (3.4+/-2.5 microgram/L) (p<0.01). However, the plasma PAI-1 in COPD patients (29.6+/-20.7 ng/mL) was similar to that in the controls. The plasma TAT showed a significant inverse relationship with the RVEF measured by the cardiac MDCT in COPD patients (r=-0.645, p<0.01). However, the plasma PAI-1 did not show a relationship with the RVEF (r=0.022, p=0.92).
CONCLUSION
These results suggest that the coagulation system in COPD patients is markedly activated, and that the plasma level of TAT might be a marker of a right ventricular dysfunction in COPD patients.
Keyword
MeSH Terms
-
Cell Proliferation
Fibrinolysis*
Humans
Hypertension, Pulmonary
Immunoassay
Multidetector Computed Tomography
Physiology
Plasma
Plasminogen Activator Inhibitor 1
Plasminogen Activators
Pulmonary Disease, Chronic Obstructive*
Smoke
Stroke Volume
Thrombin
Thromboembolism
Tobacco
Vasoconstriction
Vasodilation
Ventricular Dysfunction, Right*
Ventricular Function, Right
Plasminogen Activator Inhibitor 1
Plasminogen Activators
Smoke
Thrombin
Figure
Reference
-
1. Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J. 1977. 1:1645–1648.2. Kim DS, Kim YS, Jung KS, Chang JH, Lim CM, Lew WJ, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005. 172:842–847.3. Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden Study. Lancet. 1997. 349:1269–1276.4. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997. 349:1498–1504.5. Hansel TT, Barnes PJ. An atlas of chronic obstructive pulmonary disease COPD. 2004. 1st ed. New York: Parthenon Publishing;56–57.6. Wright JL, Levy RD, Churg A. Pulmonary hypertension in chronic obstructive pulmonary disease: current theories of pathogenesis and their implication for treatment. Thorax. 2005. 60:605–609.7. Lopes AA, Caramuru LH, Maeda NY. Endothelial dysfunction associated with chronic intravascular coagulation in secondary pulmonary hypertension. Clin Appl Thromb Hemost. 2002. 8:353–358.8. Hoeper MM, Sosada M, Fabel H. Plasma coagulation profiles in patients with severe primary pulmonary hypertension. Eur Respir J. 1998. 12:1446–1449.9. Wedzicha JA, Seemungal TA, MacCallum PK, Paul EA, Donaldson GC, Bhowmik A, et al. Acute exacerbations of chronic obstructive pulmonary disease are accompanied by elevations of plasma fibrinogen and IL-6 levels. Thromb Haemost. 2000. 84:210–215.10. Ashitani J, Mukae H, Arimura Y, Matsukura S. Elevated plasma procoagulant and fibrinolytic markers in patients with chronic obstructive pulmonary disease. Intern Med. 2002. 41:181–185.11. Kim TH, Ryu YH, Hur J, Kim SJ, Kim HS, Choi BW, et al. Evaluation of right ventricular volume and mass using retrospective cardiac multidetector computer tomography: comparison with first-pass radionuclide angiography. Eur Radiol. 2005. 15:1987–1993.12. Park KJ, Kim HJ, Hwang SC, Lee SM, Lee YH, Hahn MH, et al. The imbalance between coagulation and fibrinolysis is related to the severity of the illness and the prognosis in sepsis. Korean J Intern Med. 1999. 14:72–77.13. Naeije R. Pulmonary hypertension and right heart failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:20–22.14. Naeije R, Barbera JA. Pulmonary hypertension associated with COPD. Crit Care. 2001. 5:286–289.15. Presberg KW, Dincer HE. Pathophysiology of pulmonary hypertension due to lung disease. Curr Opin Pulm Med. 2003. 9:131–138.16. Eisenberg PR, Lucore C, Kaufman L, Sobel BE, Jaffe AS, Rich S. Fibrinopeptide A level indicate of pulmonary vascular thrombosis with primary pulmonary hypertension. Circulation. 1990. 82:841–847.17. Christ G, Graf S, Huber-Beckmann R, Zorn G, Lang I, Kneussi M, et al. Impairment of the plasmin activation system in primary pulmonary hypertension: evidence for gender differences. Thromb Haemos. 2001. 86:557–562.18. Alessandri C, Basili S, Violi F, Ferroni P, Gazzaniga PP, Cordova C. Hypercoagulability state in patients with chronic obstructive pulmonary disease. Thromb Haemost. 1994. 72:343–346.19. Altman R, Scazziota A, Rouvier J, Gurfinkel E, Favaloro R, Perrone S, et al. Coagulation and fibrinolytic parameters in patients with pulmonary hypertension. Clin Cardiol. 1996. 19:549–554.20. Kruithof EK, Baker MS, Bunn CL. Biological and clinical aspects of plasminogen activator inhibitor type 2. Blood. 1995. 86:4007–4024.21. Huber K, Rosc D, Resch I, Schuster E, Glogar DH, Kaindl F, et al. Circadian fluctuations of plasminogen activator inhibitor and tissue plasminogen activator levels in plasma of patients with unstable coronary artery disease and acute myocardial infarction. Thromb Haemost. 1988. 60:372–376.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Echocardiographic Evaluation of Right Ventricular Diastolic Function in Patients with Chronic Obstructive Pulmonary Disease
- Studies on the Systolic Time Intervals in the Patients with COPD
- Observation of Cardiac Arrhythmias in Hospitalized Patients with Chronic Obstructive Pulmonary Disease by 24-Hour Continuous Ambulating Electrocardiographic Recording
- Assessment of Right Ventricular Function in Patients with Chronic Obstructive Pulmonary Disease Using Echocardiographic Tei Index
- Cor Pulmonale with Particular Reference to Chronic Obstructive Pulmonary Disease and Pulmonary Tuberculosis