Endocrinol Metab.
2012 Jun;27(2):138-141. 10.3803/EnM.2012.27.2.138.
Langerhans Cell Histiocytosis in the Thyroid and Draining Lymph Nodes: A Case Report
- Affiliations
-
- 1Department of Pathology, Gachon University School of Medicine, Incheon, Korea.
- 2Department of Surgery, Gachon University School of Medicine, Incheon, Korea.
- 3Department of Pathology, Ewha Womans University School of Medicine, Seoul, Korea. spark0430@ewha.ac.kr
- KMID: 1497653
- DOI: http://doi.org/10.3803/EnM.2012.27.2.138
Abstract
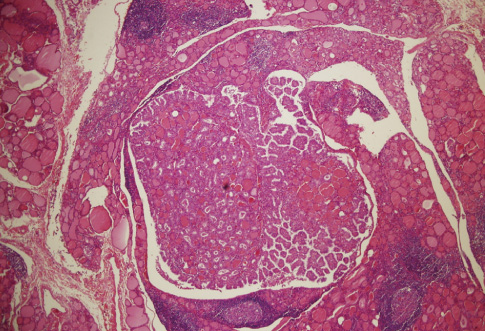
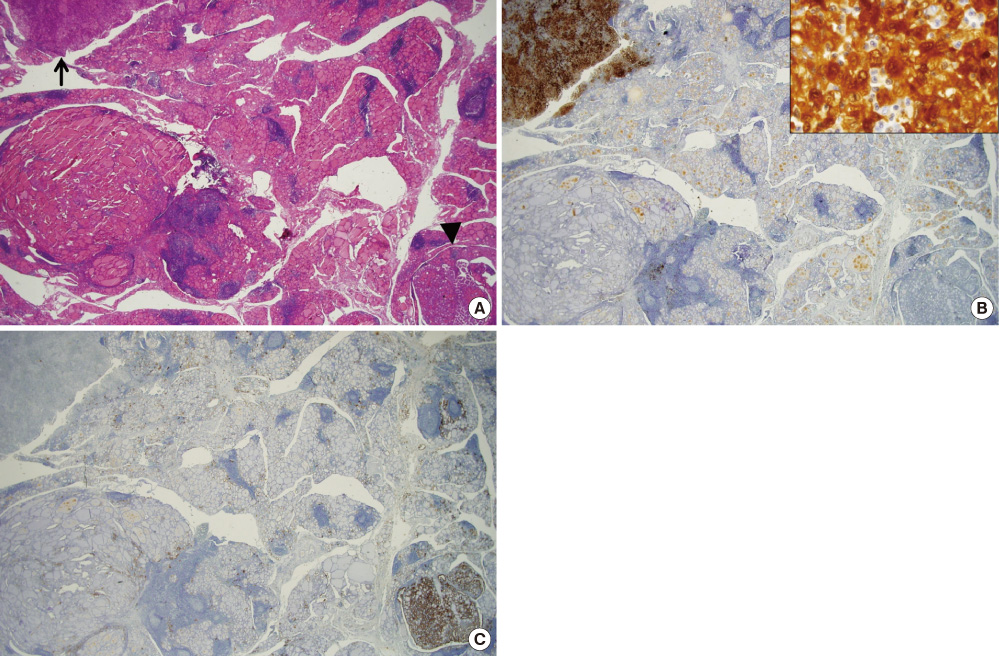
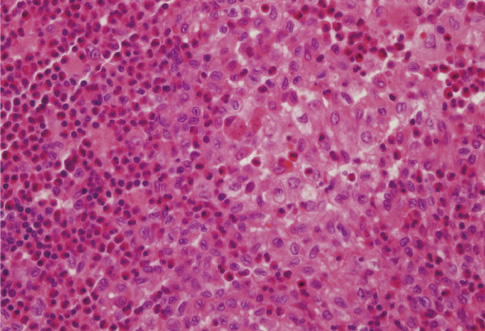
- A 53-year-old woman was presented with several 0.3-0.6 cm-sized nodules within the right lobe of the thyroid. Histologic sections of the thyroid demonstrated multiple papillary microcarcinomas in the background of lymphocytic thyroiditis, with a small focus of Langerhans cell histiocytosis (LCH). Small LCH nodules were also found in the draining cervical lymph nodes. Although the association of LCH with papillary thyroid carcinoma in the thyroid has been reported, their co-existence with LCH in the draining lymph nodes is very rare.
MeSH Terms
Figure
Reference
-
1. Favara BE, Feller AC, Pauli M, Jaffe ES, Weiss LM, Arico M, Bucsky P, Egeler RM, Elinder G, Gadner H, Gresik M, Henter JI, Imashuku S, Janka-Schaub G, Jaffe R, Ladisch S, Nezelof C, Pritchard J. Contemporary classification of histiocytic disorders. The WHO Committee on histiocytic/ reticulum cell proliferations. Reclassification Working Group of the Histiocyte Society. Med Pediatr Oncol. 1997. 29:157–166.2. Fleming MD, Pinkus JL, Fournier MV, Alexander SW, Tam C, Loda M, Sallan SE, Nichols KE, Carpentieri DF, Pinkus GS, Rollins BJ. Coincident expression of the chemokine receptors CCR6 and CCR7 by pathologic Langerhans cells in Langerhans cell histiocytosis. Blood. 2003. 101:2473–2475.3. Egeler RM, Neglia JP, Puccetti DM, Brennan CA, Nesbit ME. Association of Langerhans cell histiocytosis with malignant neoplasms. Cancer. 1993. 71:865–873.4. Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer. 1999. 85:2278–2290.5. Coode PE, Shaikh MU. Histiocytosis X of the thyroid masquerading as thyroid carcinoma. Hum Pathol. 1988. 19:239–241.6. Saiz E, Bakotic BW. Isolated Langerhans cell histiocytosis of the thyroid: a report of two cases with nuclear imaging-pathologic correlation. Ann Diagn Pathol. 2000. 4:23–28.7. Burnett A, Carney D, Mukhopadhyay S, Scalzetti EM, Leino D, Souid AK. Thyroid involvement with Langerhans cell histiocytosis in a 3-year-old male. Pediatr Blood Cancer. 2008. 50:726–727.8. Foulet-Rogé A, Josselin N, Guyetant S, Gardet JJ, Besancon A, Saint-André JP, Fabiani B. Incidental langerhans cell histiocytosis of thyroid: case report and review of the literature. Endocr Pathol. 2002. 13:227–233.9. Goldstein N, Layfield LJ. Thyromegaly secondary to simultaneous papillary carcinoma and histiocytosis X. Report of a case and review of the literature. Acta Cytol. 1991. 35:422–426.10. Thompson LD, Wenig BM, Adair CF, Smith BC, Heffess CS. Langerhans cell histiocytosis of the thyroid: a series of seven cases and a review of the literature. Mod Pathol. 1996. 9:145–149.11. Vergez S, Rouquette I, Ancey M, Serrano E, Caron P. Langerhans cell histiocytosis of the thyroid is a rare entity, but an association with a papillary thyroid carcinoma is often described. Endocr Pathol. 2010. 21:274–276.12. Lindley R, Hoile R, Schofield J, Ashton-Key M. Langerhans cell histiocytosis associated with papillary carcinoma of the thyroid. Histopathology. 1998. 32:180.13. Safali M, McCutcheon JM, Wright DH. Langerhans cell histiocytosis of lymph nodes: draining a papillary carcinoma of the thyroid. Histopathology. 1997. 30:599–603.14. Schofield JB, Alsanjari NA, Davis J, MacLennan KA. Eosinophilic granuloma of lymph nodes associated with metastatic papillary carcinoma of the thyroid. Histopathology. 1992. 20:181–183.15. Lee KW, Chung CK, Hwang SC, Yim HH, Park SY, Lee SK, Chung YS, Kim HM, Kim YJ, Hong EK, Chae BN. A case with multifocal Langerhans cell granulomatosis involving the thyroid gland. J Korean Soc Endocrinol. 1998. 13:466–472.16. Hoover KB, Rosenthal DI, Mankin H. Langerhans cell histiocytosis. Skeletal Radiol. 2007. 36:95–104.17. Stockschlaeder M, Sucker C. Adult Langerhans cell histiocytosis. Eur J Haematol. 2006. 76:363–368.18. Lieberman PH, Jones CR, Steinman RM, Erlandson RA, Smith J, Gee T, Huvos A, Garin-Chesa P, Filippa DA, Urmacher C, Gangi MD, Sperber M. Langerhans cell (eosinophilic) granulomatosis. A clinicopathologic study encompassing 50 years. Am J Surg Pathol. 1996. 20:519–552.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report
- Fine Needle Aspiration Cytology of Langerhans' Cell Histiocytosis in the Lymph Node
- Isolated Thymic Langerhans Cell Histiocytosis
- A Case of Langerhans Cell Histiocytosis in an Adult
- Multiple langerhans cell histiocytosis at the lung and mandible: Case report