Tuberc Respir Dis.
2013 Apr;74(4):191-194. 10.4046/trd.2013.74.4.191.
Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium chelonae: A Case Report
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wjkoh@skku.edu
- 2Department of Microbiology, Chungnam National University College of Medicine, Daejeon, Korea.
- 3Department of Microbiology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1495861
- DOI: http://doi.org/10.4046/trd.2013.74.4.191
Abstract
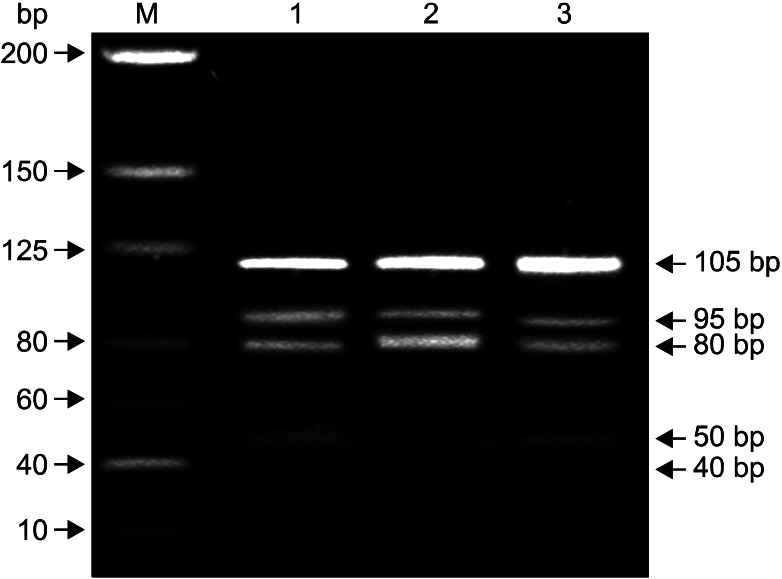
- Mycobacterium chelonae lung disease is very rare. We report a case of lung disease caused by M. chelonae in a previously healthy woman. A 69-year-old woman was referred to our hospital because of hemoptysis. A computed tomography (CT) scan of the chest revealed bronchiolitis associated with bronchiectasis in the lingular division of the left upper lobe. Nontuberculous mycobacteria were isolated three times from sputum specimens. All isolates were identified as M. chelonae by various molecular methods that characterized rpoB and hsp65 gene sequences. Although some new lesions including bronchiolitis in the superior segment of the left lower lobe developed on the chest CT scan 35 months after diagnosis, she has been followed up without antibiotic therapy because of her mild symptoms. To the best of our knowledge, this is the first case of M. chelonae lung disease in Korea in which the etiologic organisms were confirmed using molecular techniques.
MeSH Terms
Figure
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416. PMID: 17277290.
Article2. Daley CL, Griffith DE. Pulmonary disease caused by rapidly growing mycobacteria. Clin Chest Med. 2002; 23:623–632. PMID: 12370998.
Article3. Colombo RE, Olivier KN. Diagnosis and treatment of infections caused by rapidly growing mycobacteria. Semin Respir Crit Care Med. 2008; 29:577–588. PMID: 18810691.
Article4. Wallace RJ Jr, Swenson JM, Silcox VA, Good RC, Tschen JA, Stone MS. Spectrum of disease due to rapidly growing mycobacteria. Rev Infect Dis. 1983; 5:657–679. PMID: 6353528.
Article5. Griffith DE, Girard WM, Wallace RJ Jr. Clinical features of pulmonary disease caused by rapidly growing mycobacteria: an analysis of 154 patients. Am Rev Respir Dis. 1993; 147:1271–1278. PMID: 8484642.
Article6. Singh N, Yu VL. Successful treatment of pulmonary infection due to Mycobacterium chelonae: case report and review. Clin Infect Dis. 1992; 14:156–161. PMID: 1571422.7. Goto T, Hamaguchi R, Maeshima A, Oyamada Y, Kato R. Pulmonary resection for Mycobacterium chelonae infection. Ann Thorac Cardiovasc Surg. 2012; 18:128–131. PMID: 22001214.8. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000; 38:2966–2971. PMID: 10921960.9. Benson DA, Karsch-Mizrachi I, Lipman DJ, Ostell J, Wheeler DL. GenBank. Nucleic Acids Res. 2007; 35:D21–D25. PMID: 17202161.
Article10. Adekambi T, Drancourt M. Dissection of phylogenetic relationships among 19 rapidly growing Mycobacterium species by 16S rRNA, hsp65, sodA, recA and rpoB gene sequencing. Int J Syst Evol Microbiol. 2004; 54(Pt 6):2095–2105. PMID: 15545441.11. Kusunoki S, Ezaki T. Proposal of Mycobacterium peregrinum sp. nov., nom. rev., and elevation of Mycobacterium chelonae subsp. abscessus (Kubica et al.) to species status: Mycobacterium abscessus comb. nov. Int J Syst Bacteriol. 1992; 42:240–245. PMID: 1581184.12. Lee MR, Keng LT, Shu CC, Lee SW, Lee CH, Wang JY, et al. Risk factors for Mycobacterium chelonae-abscessus pulmonary disease persistence and deterioration. J Infect. 2012; 64:228–230. PMID: 22101165.13. Scarparo C, Piccoli P, Rigon A, Ruggiero G, Nista D, Piersimoni C. Direct identification of mycobacteria from MB/BacT alert 3D bottles: comparative evaluation of two commercial probe assays. J Clin Microbiol. 2001; 39:3222–3227. PMID: 11526154.
Article14. Hazelton TR, Newell JD Jr, Cook JL, Huitt GA, Lynch DA. CT findings in 14 patients with Mycobacterium chelonae pulmonary infection. AJR Am J Roentgenol. 2000; 175:413–416. PMID: 10915685.15. Nash KA, Brown-Elliott BA, Wallace RJ Jr. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob Agents Chemother. 2009; 53:1367–1376. PMID: 19171799.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium chelonae Infection at the Site of Acupuncture
- Nontuberculous Mycobacterial Pulmonary Diseases in Immunocompetent Patients
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium shinjukuense: The First Reported Case in Korea
- Respiratory Review of 2009: Nontuberculous Mycobacterium
- Mycobacterium chelonae Skin Infection after Autologous Fat Transplantation