Korean J Radiol.
2013 Apr;14(2):287-293. 10.3348/kjr.2013.14.2.287.
Accuracy of Preoperative MRI with Microscopy Coil in Evaluation of Primary Tumor Thickness of Malignant Melanoma of the Skin with Histopathologic Correlation
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul 110-744, Korea. jacrad@radiol.snu.ac.kr
- 2Department of Radiology, Seoul National University Bundang Hospital, Seongnam 463-707, Korea.
- 3Department of Pathology, Seoul National University Bundang Hospital, Seongnam 463-707, Korea.
- KMID: 1482789
- DOI: http://doi.org/10.3348/kjr.2013.14.2.287
Abstract
OBJECTIVE
The purpose of this study was to evaluate the accuracy of a preoperative MRI with microscopy coils in determining the primary tumor thickness of malignant melanoma with histopathologic correlation.
MATERIALS AND METHODS
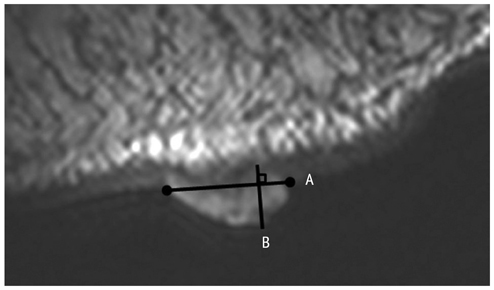
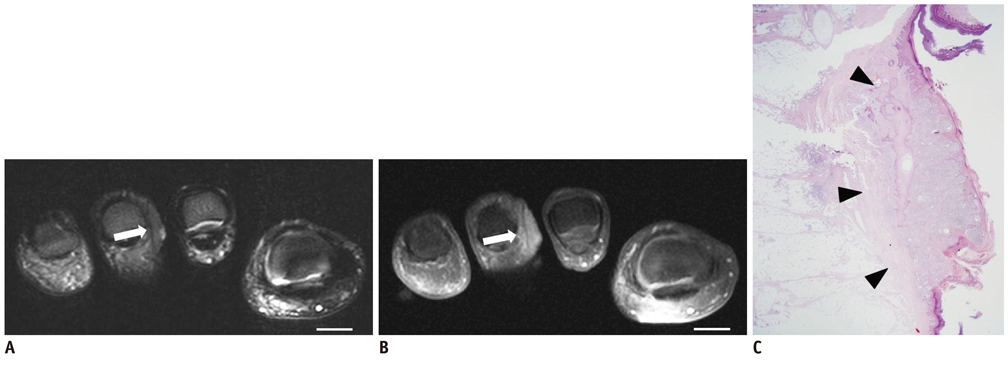
Eleven patients with histopathologically confirmed malignant melanoma were included in this study. MR images of the tumors were obtained with a 47-mm microscopy coil on 1.5T MR scanners and were evaluated by two radiologists, who assessed the thickness of the primary tumor on T2-weighted images (T2WI) and gadolinium-enhanced T1-weighted images with fat suppression (Gd-T1WI) and compared the results with the histopathologic findings as the reference standard. Correlations between tumor thickness on MRI and histopathologic examination were assessed using concordance correlation coefficients (CCCs). Inter- and intraobserver variabilities of tumor measurements were also assessed by intraclass correlation coefficient (ICC).
RESULTS
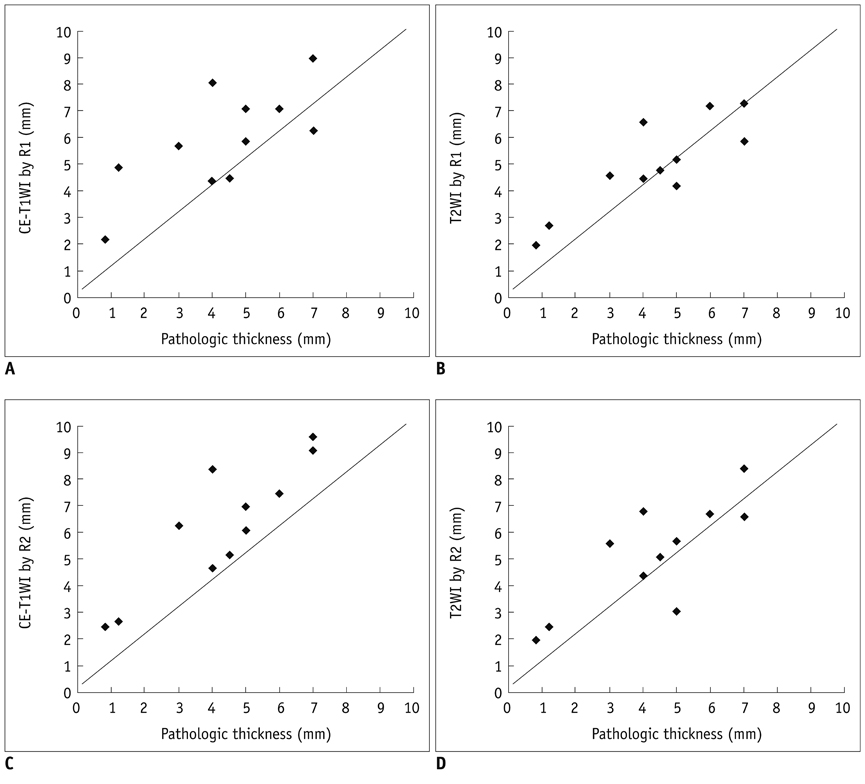
Among the 11 cases included in the study, 10 cases from the same number of patients were managed with surgical excision and one case was confirmed with punch biopsy. The primary tumor thickness measured on T2WI showed better correlation with histopathologic results, as compared with measurements taken on Gd-T1WI: the CCC of measurements on T2WI ranged from 0.64 to 0.78, indicating a substantial agreement, whereas the CCC of measurements on Gd-T1WI ranged from 0.50 to 0.61, indicating a moderate to substantial agreement. Inter- and intraobserver agreements of readers 1 and 2 were excellent for both T2WI and Gd-T1WI, with ICC ranging from 0.86 to 0.99.
CONCLUSION
MR imaging with microscopy coils may be an accurate technique in the preoperative assessment of tumor thickness in malignant melanoma, especially on T2-weighted images.
Keyword
MeSH Terms
Figure
Reference
-
1. Rajeswari MR, Jain A, Sharma A, Singh D, Jagannathan NR, Sharma U, et al. Evaluation of skin tumors by magnetic resonance imaging. Lab Invest. 2003. 83:1279–1283.2. Kim HJ, Lee SH, Kang CH, Ryu JA, Shin MJ, Cho KJ, et al. Evaluation of the chondromalacia patella using a microscopy coil: comparison of the two-dimensional fast spin echo techniques and the three-dimensional fast field echo techniques. Korean J Radiol. 2011. 12:78–88.3. Georgouli T, James T, Tanner S, Shelley D, Nelson M, Chang B, et al. High-resolution microscopy coil MR-Eye. Eye (Lond). 2008. 22:994–996.4. Lee IS, Choi JA, Oh JH, Chung JH, Jeong HS, Hong SH, et al. Microscopy coil for preoperative MRI of small soft-tissue masses of the hand and foot: comparison with conventional surface coil. AJR Am J Roentgenol. 2008. 191:W256–W263.5. Maderwald S, Ladd SC, Ladd ME, Stock F, Paul T, Liffers A, et al. High SNR, Microscopic Imaging of Skin Lesions. Proc Intl Soc Mag Reson Med. 2006. 14:1737.6. Mäurer J, Knollmann FD, Schlums D, Garbe C, Vogl TJ, Bier J, et al. Role of high-resolution magnetic resonance imaging for differentiating melanin-containing skin tumors. Invest Radiol. 1995. 30:638–643.7. Pennasilico GM, Arcuri PP, Laschena F, Potenza C, Ruatti P, Bono R, et al. Magnetic resonance imaging in the diagnosis of melanoma: in vivo preliminary studies with dynamic contrast-enhanced subtraction. Melanoma Res. 2002. 12:365–371.8. Balch CM, Murad TM, Soong SJ, Ingalls AL, Halpern NB, Maddox WA. A multifactorial analysis of melanoma: prognostic histopathological features comparing Clark's and Breslow's staging methods. Ann Surg. 1978. 188:732–742.9. Ivan D, Prieto VG. An update on reporting histopathologic prognostic factors in melanoma. Arch Pathol Lab Med. 2011. 135:825–829.10. Büsing KA, Kilian AK, Schaible T, Debus A, Weiss C, Neff KW. Reliability and validity of MR image lung volume measurement in fetuses with congenital diaphragmatic hernia and in vitro lung models. Radiology. 2008. 246:553–561.11. Kim SY, Lee SS, Byun JH, Park SH, Kim JK, Park B, et al. Malignant hepatic tumors: short-term reproducibility of apparent diffusion coefficients with breath-hold and respiratory-triggered diffusion-weighted MR imaging. Radiology. 2010. 255:815–823.12. Mazaheri Y, Hricak H, Fine SW, Akin O, Shukla-Dave A, Ishill NM, et al. Prostate tumor volume measurement with combined T2-weighted imaging and diffusion-weighted MR: correlation with pathologic tumor volume. Radiology. 2009. 252:449–457.13. Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989. 45:255–268.14. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33:159–174.15. Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009. 27:6199–6206.16. Veronesi U, Cascinelli N. Narrow excision (1-cm margin). A safe procedure for thin cutaneous melanoma. Arch Surg. 1991. 126:438–441.17. Veronesi U, Cascinelli N, Adamus J, Balch C, Bandiera D, Barchuk A, et al. Thin stage I primary cutaneous malignant melanoma. Comparison of excision with margins of 1 or 3 cm. N Engl J Med. 1988. 318:1159–1162.18. Krug B, Kugel H, Schulze HJ, Krahe T, Gieseke J, Lackner K. High-resolution MR imaging of the cutis and subcutis. Histological correlation. Acta Radiol. 1998. 39:547–553.19. Gufler H, Franke FE, Rau WS. High-resolution MRI of basal cell carcinomas of the face using a microscopy coil. AJR Am J Roentgenol. 2007. 188:W480–W484.20. Kalli S, Freer PE, Rafferty EA. Lesions of the skin and superficial tissue at breast MR imaging. Radiographics. 2010. 30:1891–1913.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidermotropic Metastatic Melanoma Clinically Resembling Agminated Spitz Nevi
- A Case report of Primary Malignant Melanoma of the Uterine Cervix
- Two Cases of Malignant Melanoma Diagnosed by MRI
- Primary Intradural Extramedullary Malignant Melanoma in the Thoracic Spine: Case Report and Literature Review
- A Case of Primary Malignant Leptomeningeal Melanoma of the Spinal Cord: Case Report