Tuberc Respir Dis.
2008 Jul;65(1):57-60. 10.4046/trd.2008.65.1.57.
Air in the Left Brachiocephalic Vein Accompanied with Pulmonary Edema
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea, College of Medicine, Seoul, Korea. mdlee@catholic.ac.kr
- KMID: 1478219
- DOI: http://doi.org/10.4046/trd.2008.65.1.57
Abstract
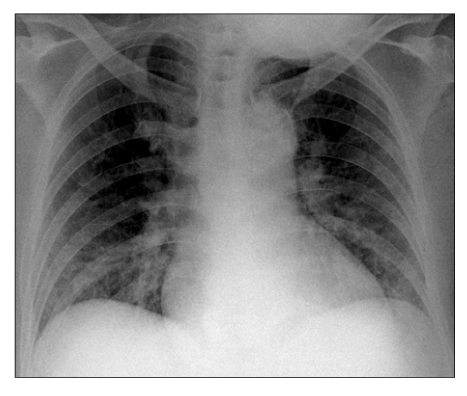
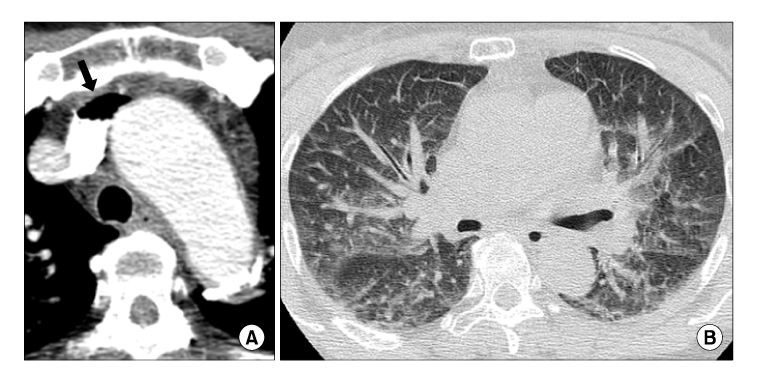
- A fifty-seven year old female patient visited the emergency department with tachypnea and a decreased mental status. The patient had been receiving fluid therapy at home and a bolus of air was injected into the fluid bottle in order to increase the infusion speed. Chest computed tomography revealed air in the left brachiocephalic vein that was accompanied with pulmonary edema the diagnosis of venous air embolism was made. Venous air embolism can result from various procedures that are performed in almost all clinical specialties and they can be fatal in cases of massive air embolism. Therefore, it is important for all clinicians to be aware of this problem.
Keyword
MeSH Terms
Figure
Reference
-
1. Muth CM, Shank ES. Gas embolism. N Engl J Med. 2000. 342:476–482.2. van Hulst RA, Klein J, Lachmann B. Gas embolism: pathophysiology and treatment. Clin Physiol Funct Imaging. 2003. 23:237–246.3. Park BC, Kil H, Park CS, Jeong JI, Choi EY, Shin YM, et al. A case of massive air embolism after contrast-enhanced computed tomography. Tuberc Respir Dis. 2007. 63:178–182.4. Groell R, Schaffler GJ, Rienmueller R, Kern R. Vascular air embolism: location, frequency, and cause on electron-beam CT studies of the chest. Radiology. 1997. 202:459–462.5. Palmon SC, Moore LE, Lundberg J, Toung T. Venous air embolism: a review. J Clin Anesth. 1997. 9:251–257.6. Elliot DH, Moon RE. Bennett PB, Elliot DH, editors. Manifestations of decompression disorders. The physiology and medicine of diving. 1996. 4th ed. Philadelphia: Saunders;481–505.7. Gildenberg PL, O'Brien RP, Britt WJ, Frost EA. The efficacy of Doppler monitoring for the detection of venous air embolism. J Neurosurg. 1981. 54:75–78.8. Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: a critical appraisal. Br J Anaesth. 1999. 82:117–128.9. Mammoto T, Hayashi Y, Ohnishi Y, Kuro M. Incidence of venous and paradoxical air embolism in neurosurgical patients in the sitting position: detection by transesophageal echocardiography. Acta Anaesthesiol Scand. 1998. 42:643–647.10. Pham KL, Cohen AJ. Iatrogenic venous air embolism during contrast enhanced computed tomography: a report of two cases. Emerg Radiol. 2003. 10:147–151.11. Lachmann B, Eijking EP, So KL, Gommers D. In vivo evaluation of the inhibitory capacity of human plasma on exogenous surfactant function. Intensive Care Med. 1994. 20:6–11.12. Frim DM, Wollman L, Evans AB, Ojemann RG. Acute pulmonary oedema after low level air embolism during craniotomy. Case report. J Neurosurg. 1996. 85:937–940.13. Van Liew HD, Conkin J, Burkard ME. The oxygen window and decompression bubbles: estimates and significance. Aviat Space Environ Med. 1993. 64:859–865.14. De Angelis J. A simple and rapid method for evacuation of embolized air. Anesthesiology. 1975. 43:110–111.15. Albin MS. Albin MS, editor. Air embolism. Textbook of neuroanesthesia with neurosurgical and neuroscience perspectives. 1997. 1st ed. New York: McGraw-Hill;1009–1025.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circumaortic Left Brachiocephalic Vein: CT Findings
- Double Left Brachiocephalic Veins with Persistent Left Superior Vena Cava: A Case Report
- An Unusual Cause of Left Brachiocephalic Vein Occlusion: Extrinsic Compression by the Aortic Arch in a Hemodialysis Patient
- Subaortic Left Brachiocephalic Vein
- Anomalous Pulmonary Venous Return Accompanied by Normal Superior Pulmonary Veins in the Left Upper Lobe: A Case Report