Tuberc Respir Dis.
2008 Jan;64(1):52-56. 10.4046/trd.2008.64.1.52.
A Case of Pheochromocytoma that Initially Presented as Diffuse Alveolar Hemorrhage
- Affiliations
-
- 1Department of Radiology, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. jbh@gnah.co.kr
- KMID: 1478143
- DOI: http://doi.org/10.4046/trd.2008.64.1.52
Abstract
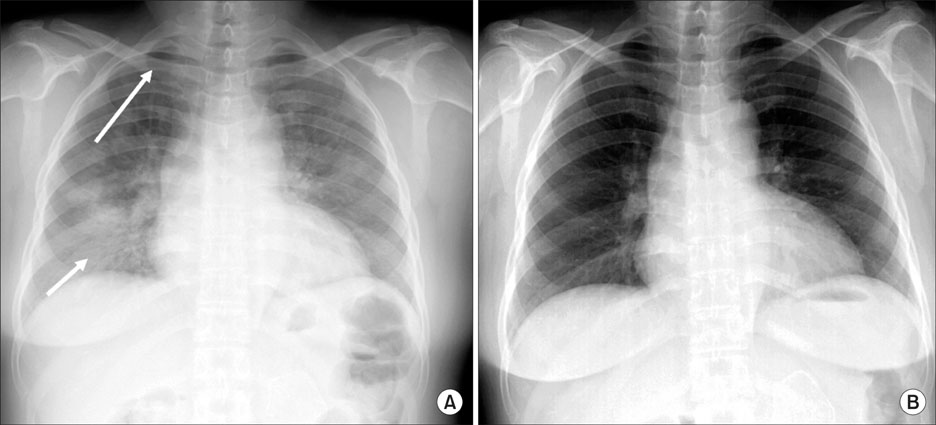
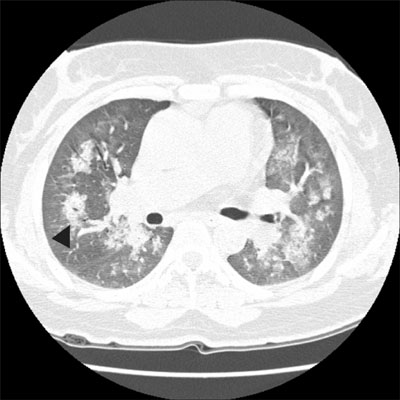
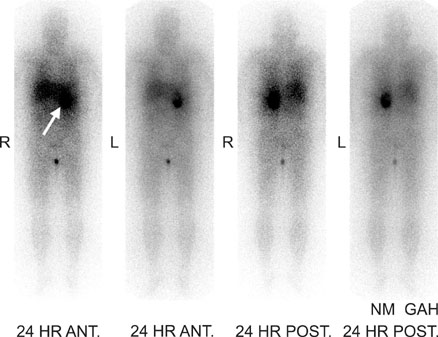
- A pheochromocytoma is a neuroectodermal tumor that originates from the chromaffin cells of the sympathetic system. Typical symptoms or signs are periodic attacks of paroxysmal hypertension, spell, palpitation, headache and sweating. However, the clinical presentation is quite variable. Therefore, an atypical clinical presentation sometimes makes a diagnosis difficult. Hemoptysis as a presenting symptom is very rare in pheochromocytoma. We recently experienced a patient with diffuse alveolar hemorrhage due to pheochromocytoma. A chest PA showed diffuse consolidation and ground glass opacities in both lungs. A chest CT showed diffuse consolidation and ground glass opacities in the central, middle and lower portion predominance of the lungs, sparing the costophrenic angles and apices of the lungs. In Korea, a case of pheochromocytoma that presented initially as massive hemoptysis due to diffuse alveolar hemorrhage has not been previously reported. We report the case with a review of the literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Frymoyer PA, Anderson GH Jr, Blair DC. Hemoptysis as a presenting symptom of pheochromocytoma. J Clin Hypertens. 1986. 2:65–67.2. Kimura Y, Ozawa H, Igarashi M, Iwamoto T, Nishiya K, Urano T, et al. A pheochromocytoma causing limited coagulopathy with hemoptysis. Tokai J Exp Clin Med. 2005. 30:35–39.3. Colas JL. Paroxysmal hypertension with haemoptysis due to a retroperitoneal paraganglioma. East Afr Med J. 1965. 42:535–540.4. Iino S, Nagashima N, Akiba H, Ban Ymiyamoto M. Hemoptysis and palpitation (with hypertension): pheochromocytoma. Nippon Rinsho. 1975. Spec No:918–919. 1394–1395.5. Bourvis N, Fartoukh M, Christin-Maitre S, Francois T, Parrot A, Mayaud C. Intra-alveolar hemorrhage revealing pheochromocytoma. Rev Pneumol Clin. 2006. 62:43–48.6. Jung YS, Kim JG, Song SK, Kwon SK, Choi YS, Jang TW, et al. A case of pheochromocytoma accompanied with hemoptysis. Kosin Med J. 2000. 15:103–107.7. Amstrong P, Wilson AG, Dee P, Hansell DM. Imaging of disease of the chest. 2000. 3rd ed. London: Mosby;582–586.8. Blake MA, Kalra MK, Maher MM, Sahani DV, Sweeney AT, Mueller PR, et al. Pheochromocytoma: an imaging chameleon. Radiographics. 2004. 24:S87–S99.9. Albelda SM, Gefter WB, Epstein DM, Miller WT. Diffuse pulmonary hemorrhage: a review and classification. Radiology. 1985. 154:289–297.10. Rossi SE, Erasmus JJ, Volpacchio M, Franquet T, McAdams HP. "Crazy-paving pattern" at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2003. 23:1509–1519.11. Primack SL, Miller RR, Müller NL. Diffuse pulmonary hemorrhage: clinical, pathologic, and imaging features. AJR Am J Roentgenol. 1995. 164:295–300.12. Webb WR, Müller NL, Naidich DP. High resolution CT of the lung. 2001. 3rd ed. Philadelphia: Lippincott Willams & Wilkins;408–409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of diffuse alveolar hemorrhage with thoracocervicofacial purpura after a generalized tonic-clonic seizure
- A Case of Microscopic Polyangiitis Presenting As Diffuse Alveolar Hemorrhage
- An Unusual Radiologic Manifestation of Pulmonary Tuberculosis with Bilateral Multiple Lung Nodules and Diffuse Alveolar Hemorrhage: A Case Report
- Interstitial Lung Disease and Diffuse Alveolar Hemorrhage, the Two Key Pulmonary Manifestations in Microscopic Polyangiitis
- Acute respiratory failure due to diffuse alveolar hemorrhage in mycoplasma pneumonia