J Clin Neurol.
2010 Dec;6(4):216-220. 10.3988/jcn.2010.6.4.216.
Arteriovenous Malformation with an Occlusive Feeding Artery Coexisting with Unilateral Moyamoya Disease
- Affiliations
-
- 1Department of Neurology, Chosun University School of Medicine, Gwangju, Korea. hoowon@chosun.ac.kr
- KMID: 1462810
- DOI: http://doi.org/10.3988/jcn.2010.6.4.216
Abstract
- BACKGROUND
Arteriovenous malformations (AVMs) with vascular abnormalities, including aneurysms, have been reported frequently. However, the coexistence of AVM and unilateral moyamoya disease is rare. We report herein an AVM patient who presented with acute ischemic stroke with unilateral moyamoya disease and occlusion of the feeding artery.
CASE REPORT
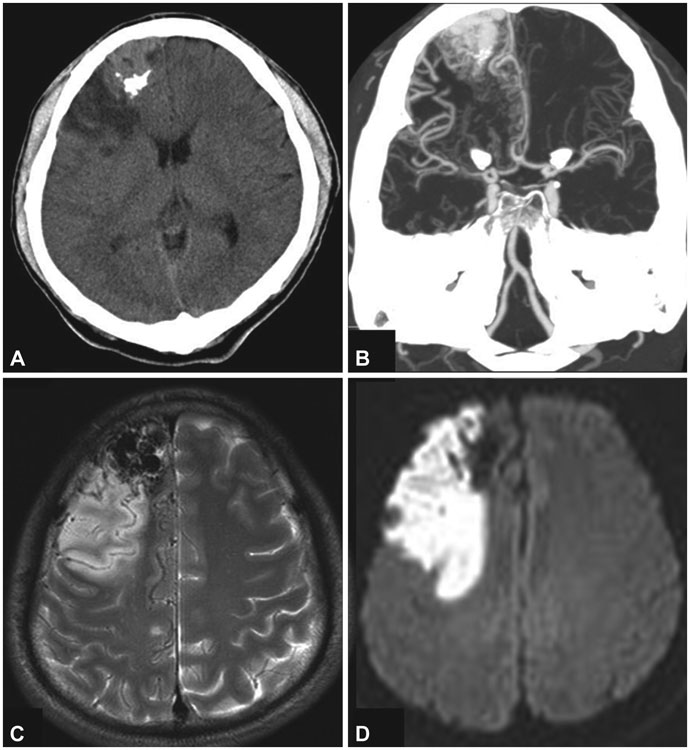
A-41-year old man was admitted with sudden dysarthria and facial palsy. Brain computed tomography and magnetic resonance imaging revealed an acute infarction adjacent to a large AVM in the right frontal lobe. Cerebral angiography revealed occlusions of the proximal right middle cerebral and proximal anterior cerebral arteries, which were the main feeders of the AVM. Innumerable telangiectatic moyamoya-type vessels between branches of the anterior cerebral artery and dilated lenticulostriate arteries on the occluded middle cerebral artery were detected. However, a nidus of the AVM was still opacified through the distal right callosomarginal artery, which was supplied by the remaining anterior cerebral artery and leptomeningeal collaterals from the posterior cerebral artery.
CONCLUSIONS
While AVM accompanied by unilateral moyamoya disease is rare, our case suggests an association between these two dissimilar vascular diseases.
MeSH Terms
Figure
Reference
-
1. Al-Shahi R, Warlow C. A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain. 2001. 124:1900–1926.
Article2. Meisel HJ, Mansmann U, Alvarez H, Rodesch G, Brock M, Lasjaunias P. Cerebral arteriovenous malformations and associated aneurysms: analysis of 305 cases from a series of 662 patients. Neurosurgery. 2000. 46:793–800.
Article3. Mullan S, Mojtahedi S, Johnson DL, Macdonald RL. Embryological basis of some aspects of cerebral vascular fistulas and malformations. J Neurosurg. 1996. 85:1–8.
Article4. Fukui M. Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis ('moyamoya' disease). Research Committee on Spontaneous Occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg. 1997. 99:Suppl 2. S238–S240.5. Enam SA, Malik GM. Association of cerebral arteriovenous malformations and spontaneous occlusion of major feeding arteries: clinical and therapeutic implications. Neurosurgery. 1999. 45:1105–1111.
Article6. Kayama T, Suzuki S, Sakurai Y, Nagayama T, Ogawa A, Yoshimoto T. A case of moyamoya disease accompanied by an arteriovenous malformation. Neurosurgery. 1986. 18:465–468.
Article7. Lichtor T, Mullan S. Arteriovenous malformation in moyamoya syndrome. Report of three cases. J Neurosurg. 1987. 67:603–608.8. Akiyama K, Minakawa T, Tsuji Y, Isayama K. Arteriovenous malformation associated with moyamoya disease: case report. Surg Neurol. 1994. 41:468–471.
Article9. Halatsch ME, Rustenbeck HH, Jansen J. Progression of arteriovenous malformation in moyamoya syndrome. Acta Neurochir (Wien). 1997. 139:82–85.
Article10. Vörös E, Kiss M, Hankó J, Nagy E. Moyamoya with arterial anomalies: relevance to pathogenesis. Neuroradiology. 1997. 39:852–856.
Article11. Seol HJ, Kim DG, Oh CW, Han DH. Radiosurgical treatment of a cerebral arteriovenous malformation in a patient with moyamoya disease: case report. Neurosurgery. 2002. 51:478–481.
Article12. Fassett DR, Schloesser PE, Couldwell WT. Hemorrhage from moyamoya-like vessels associated with a cerebral arteriovenous malformation. Case report. J Neurosurg. 2004. 101:869–871.
Article13. Nawawi O, Sinnasamy M, Ramli N. Unilateral moyamoya disease with co-existing arteriovenous malformation. Br J Radiol. 2006. 79:e12–e15.
Article14. Somasundaram S, Thamburaj K, Burathoki S, Gupta AK. Moyamoya disease with cerebral arteriovenous malformation presenting as primary subarachnoid hemorrhage. J Neuroimaging. 2007. 17:251–254.
Article15. Chen Z, Zhu G, Feng H, Lin J, Wu N. Giant arteriovenous malformation associated with unilateral moyamoya disease in a child: case report. Surg Neurol. 2007. 67:89–92.
Article16. Montanera W, Marotta TR, terBrugge KG, Lasjaunias P, Willinsky R, Wallace MC. Cerebral arteriovenous malformations associated with moyamoya phenomenon. Am J Neuroradiol. 1990. 11:1153–1156.17. Mawad ME, Hilal SK, Michelsen WJ, Stein B, Ganti SR. Occlusive vascular disease associated with cerebral arteriovenous malformations. Radiology. 1984. 153:401–408.
Article18. Fuse T, Takagi T, Fukushima T, Hashimoto N, Yamada K. Arteriovenous malformation associated with moyamoya disease. Childs Nerv Syst. 1996. 12:404–408.
Article19. Schmit BP, Burrows PE, Kuban K, Goumnerova L, Scott RM. Acquired cerebral arteriovenous malformation in a child with moyamoya disease. Case report. J Neurosurg. 1996. 84:677–680.
Article20. O'Shaughnessy BA, DiPatri AJ Jr, Parkinson RJ, Batjer HH. Development of a de novo cerebral arteriovenous malformation in a child with sickle cell disease and moyamoya arteriopathy. Case report. J Neurosurg. 2005. 102:238–243.21. Yoshimoto T, Houkin K, Takahashi A, Abe H. Angiogenic factors in moyamoya disease. Stroke. 1996. 27:2160–2165.
Article22. Nakashima T, Nakayama N, Furuichi M, Kokuzawa J, Murakawa T, Sakai N. Arteriovenous malformation in association with moyamoya disease. Report of two cases. Neurosurg Focus. 1998. 5:e6.23. Deng ZH, Wang S, Li Z, Zhao JZ. Unilateral moyamoya disease associated with cerebellar arteriovenous malformation: one case report. Chin Med J (Engl). 2008. 121:1145–1147.
Article24. Okada T, Kida Y, Kinomoto T, Sakurai T, Kobayashi T. Arteriovenous malformation associated with moyamoya disease--case report. Neurol Med Chir (Tokyo). 1990. 30:945–948.25. Houkin K, Abe H, Yoshimoto T, Takahashi A. Is "unilateral" moyamoya disease different from moyamoya disease? J Neurosurg. 1996. 85:772–776.
Article26. Ogata T, Yasaka M, Inoue T, Yasumori K, Ibayashi S, Iida M, et al. The clinical features of adult unilateral moyamoya disease: does it have the same clinical characteristics as typical moyamoya disease? Cerebrovasc Dis. 2008. 26:244–249.
Article27. Liebeskind DS. Collateral circulation. Stroke. 2003. 34:2279–2284.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Probable Moyamoya Disease (Unilateal Moyamoya Disease) Coexisting Arteriovenous Malformation
- Arteriovenous Malformation at Cerebellopontine Angle Associated with a Fenestration of the Vertebral Artery
- Concomitant moyamoya syndrome and infratentorial arteriovenous malformation in a neurofibromatosis type 1 patient: a case report
- A Case of Moyamoya Disease Associated with Complete Duplication of the Basilar artery
- Cerebral Arteriovenous Malformation Associated with Intracranial Meningioma and Aneurysm: Case Report