J Korean Hip Soc.
2010 Dec;22(4):319-322. 10.5371/jkhs.2010.22.4.319.
Obturator Internus Pyomyositis: A Case Report
- Affiliations
-
- 1Orthopedic Surgery & Institute for Skeletal Aging, College of Medicine, Hallym University, Chuncheon, Korea. totalhip@hallym.ac.kr
- 2Infectious Disease Medical Research Center, College of Medicine, Hallym University, Chuncheon, Korea.
- KMID: 1461188
- DOI: http://doi.org/10.5371/jkhs.2010.22.4.319
Abstract
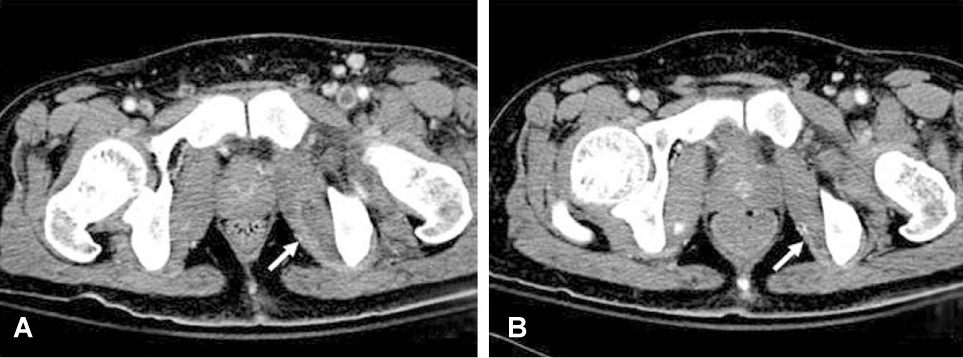
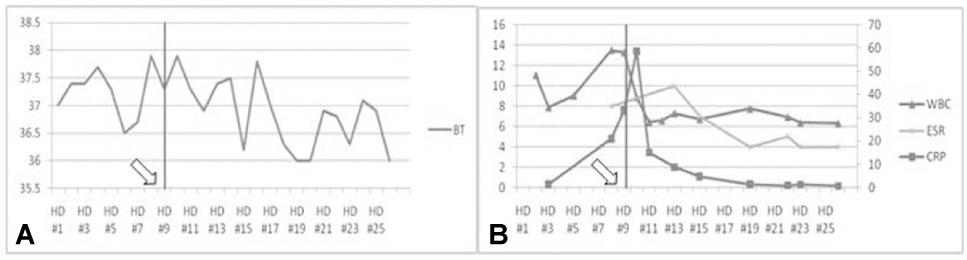
- Pyomyositis is a primary bacterial infection of skeletal muscle and this is on the increase worldwide among children as well as young adults. We report herein on a case of a 29-year-old male with pyomyositis of the obturator internus. The fact that pyomyositis predominantly affects the muscles of the lower limb and it is confined to the obturator internus muscle has been poorly recognized. CT with an enhancement was an accurate imaging modality to image the obturator internus muscle and to ascertain the diagnosis for this case. The patient was managed with antibiotics and surgical intervention was not necessary. Pyomyositis of the obturator internus muscle needs to be differentiated from septic arthritis of the hip. The present study reports the clinical signs and treatments of pyomyostis and we review the relevant literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Chiedozi LC. Pyomyositis. Review of 205 cases in 112 patients. Am J Surg. 1979. 137:255–259.2. Nikolopoulos DD, Apostolopoulos A, Polyzois I, Liarokapis S, Michos I. Obturator internus pyomyositis in a young adult: a case report and review of the literature. Cases J. 2009. 2:8588.
Article3. Birkbeck D, Watson JT. Obturator internus pyomyositis. A case report. Clin Orthop Relat Res. 1995. 316:221–226.4. Bansal M, Bhaliak V, Bruce CE. Obturator internus muscle abscess in a child: a case report. J Pediatr Orthop B. 2008. 17:223–224.
Article5. Orlicek SL, Abramson JS, Woods CR, Givner LB. Obturator internus muscle abscess in children. J Pediatr Orthop. 2001. 21:744–748.
Article6. Christin L, Sarosi GA. Pyomyositis in North America: case reports and review. Clin Infect Dis. 1992. 15:668–677.
Article7. King RJ, Laugharne D, Kerslake RW, Holdsworth BJ. Primary obturator pyomyositis: a diagnostic challenge. J Bone Joint Surg Br. 2003. 85:895–898.8. Hakim A, Graven M, Alsaeid K, Ayoub EM. Obturator internus abscess. Pediatr Infect Dis J. 1993. 12:166–168.
Article9. Chatwani A, Shapiro T, Mitra A, LevToaff A, Reece EA. Postpartum paravaginal hematoma and lower-extremity infection. Am J Obstet Gynecol. 1992. 166:598–600.10. Mazur JM, Ross G, Cummings J, Hahn GA Jr, McCluskey WP. Usefulness of magnetic resonance imaging for the diagnosis of acute musculoskeletal infections in children. J Pediatr Orthop. 1995. 15:144–147.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Imaging Features of Obturator Internus Bursa of the Hip
- Obturator Internus Myofascial Pain: A Cause of Undiagnosed Chronic Pelvic Pain Syndrome: Case reports
- Salmonella Pyomyositisina Multiple Myeloma Patient: A Case Report
- Obturator Neuropathy after Traumatic Posterior Hip Dislocation: A case report
- Contralateral Obturator Hernia Immediately after a Right Obturator Herniorrhaphy: A Case Report