J Korean Fract Soc.
2011 Jan;24(1):73-78. 10.12671/jkfs.2011.24.1.73.
Interposition of Periosteum in Distal Tibial Physeal Fractures of Children
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dongguk University, Gyeonju, Korea. kys7374@freechal.com
- KMID: 1449420
- DOI: http://doi.org/10.12671/jkfs.2011.24.1.73
Abstract
- PURPOSE
To evaluate the factors influencing periosteal interposition in distal tibial physeal fractures of children.
MATERIALS AND METHODS
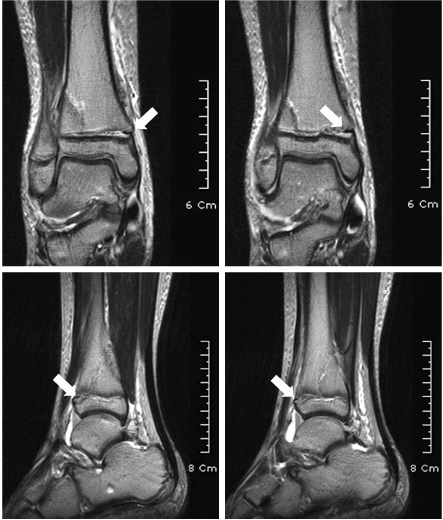
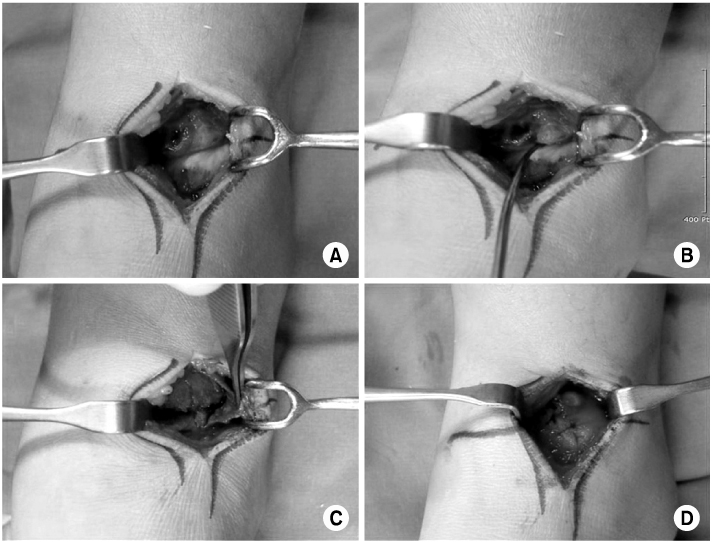
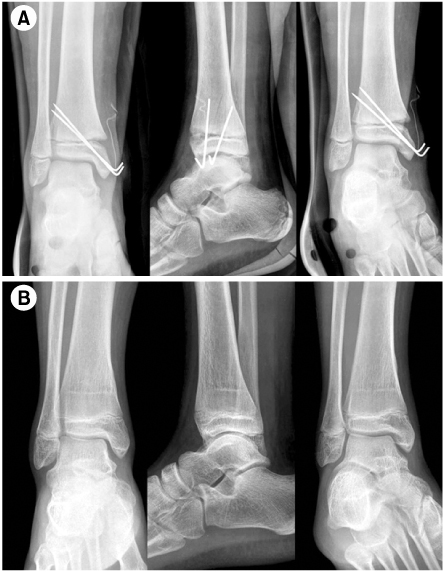
34 cases of distal tibial physeal fractures were analysed. We confirmed the presence of periosteal interposition with MRI in all cases and accessed the relationship between periosteal interposition and gender, age, cause of injury, type of fracture, degree of initial displacement and after closed reduction.
RESULTS
9 (26.5%) of 34 fractures had interposed periosteum. There was no statistically significant correlation between periosteal interposition and gender, age, cause of injury (p>0.05). 5 (83.3%) of 6 pronation-eversion-external rotation type of fractures according to Dias-Tachjian classification had interposed periosteum and that was a statistically significant correlation (p=0.006). As Salter-Harris type was toward to high degree, there were decreasing tendency of periosteal interposition (p=0.026). There was high rate of periosteal interposition in case of displacement more than 2 mm in each initial and after closed reduction (p<0.05).
CONCLUSION
There was high incidence of periosteal interposition in pronation-eversion-external rotation type with displacement more than 2 mm in distal tibial physeal fractures of children. But, periosteal interposition could occur in fractures with mild displacement less than 2 mm, if initial fracture displacement was more than 2 mm, the methods of treatment should be decided after confirm the presence of periosteal interposition with MRI after closed reduction.
Figure
Reference
-
1. Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003. 23:733–739.2. Cummings RJ. Beaty JH, Kasser JR, editors. Distal tibial and fibular fractures. Rockwood and Wilkins' fracture in children. 2006. 6th ed. Philadelphia: Lippincott, Williams & Wilkins;1077–1128.3. Dias LS, Tachdjian MO. Physeal injuries of the ankle in children: classification. Clin Orthop Relat Res. 1978. 136:230–233.4. Gruber HE, Phieffer LS, Wattenbarger JM. Physeal fractures, part II: fate of interposed periosteum in a physeal fracture. J Pediatr Orthop. 2002. 22:710–716.
Article5. Hahn SH, Yang BK, Yi SR, Yoo SH. Treatment of distal tibial epiphyseal fracture salter-harris type I & II. J Korean Soc Fract. 1999. 12:1065–1070.
Article6. Kim JR, Pyo SH, Hwang BY. Results of treatment for epiphyseal injuries of the ankle in children. J Korean Soc Fract. 2000. 13:680–685.7. Kim JR, Song KH. Factors influencing premature physeal closure following physeal injury of the ankle in children. J Korean Orthop Assoc. 2008. 43:672–676.
Article8. Kim KC, Choi JY, Kim JS, Jhe YS, Yun BC. Treatment of the pediatric ankle fracture. J Korean Soc Fract. 1996. 9:341–348.
Article9. Kling TF Jr, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. J Bone Joint Surg Am. 1984. 66:647–657.
Article10. Leary JT, Handling M, Talerico M, Yong L, Bowe JA. Physeal fractures of the distal tibia: predictive factors of premature physeal closure and growth arrest. J Pediatr Orthop. 2009. 29:356–361.11. O'Driscoll SW, Keeley FW, Salter RB. The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion. An experimental investigation in the rabbit. J Bone Joint Surg Am. 1986. 68:1017–1035.12. Phieffer LS, Meyer RA Jr, Gruber HE, Easley M, Wattenbarger JM. Effect of interposed periosteum in an animal physeal fracture model. Clin Orthop Relat Res. 2000. 376:15–25.
Article13. Rohmiller MT, Gaynor TP, Pawelek J, Mubarak SJ. Salter-Harris I and II fractures of the distal tibia: does mechanism of injury relate to premature physeal closure? J Pediatr Orthop. 2006. 26:322–328.14. Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963. 45:587–622.
Article15. Schurz M, Binder H, Platzer P, Schulz M, Hajdu S, Vécsei V. Physeal injuries of the distal tibia: long-term results in 376 patients. Int Orthop. 2010. 34:547–552.
Article16. Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula A retrospective study of two hundred and thirty-seven cases in children. J Bone Joint Surg Am. 1978. 60:1046–1050.
Article17. Weber BG. Fibrous interposition causing valgus deformity after fracture of the upper tibial metaphysis in children. J Bone Joint Surg Br. 1977. 59:290–292.
Article18. Wirth T, Byers S, Byard RW, Hopwood JJ, Foster BK. The implantation of cartilaginous and periosteal tissue into growth plate defects. Int Orthop. 1994. 18:220–228.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Findings of Periosteal Interposition in a Distal Tibial Salter-Harris Type I Fracture with Surgical Correlation: A Case Report
- Salter-Harris Type IV Physeal Fracture of the Distal Radius: A Case Report
- Triplane Fracture Management: Prediction of Periosteal Entrapment and the Need for Open Reduction by Measurements of the Physeal Fracture Gap in Preoperative Computed Tomography Scans
- Physeal and metaphyseal fractures of the distal radius in pediatric patients
- Comparison of Pediatric Distal Radius Fracture Patterns according to Age