J Korean Fract Soc.
2012 Oct;25(4):295-299. 10.12671/jkfs.2012.25.4.295.
Intermittent Parathyroid Hormone Treatment for Stimulation of Callus Formation in Elderly Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea. kyang@yuhs.ac
- 2Department of Radiology, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Orthopedic Surgery, Ajou University School of Medicine, Suwon, Korea.
- KMID: 1434069
- DOI: http://doi.org/10.12671/jkfs.2012.25.4.295
Abstract
- PURPOSE
The purpose of this study was to evaluate the effect of parathyroid hormone (PTH) on fracture healing in elderly patients.
MATERIALS AND METHODS
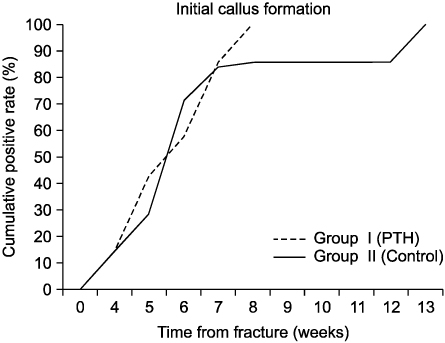
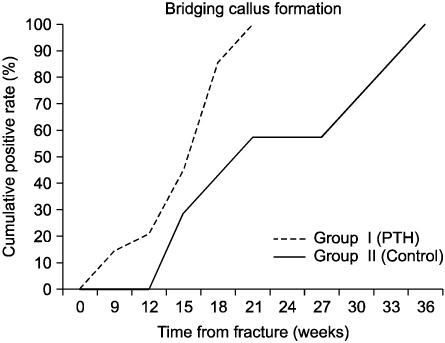
We analyzed the radiologic results in 14 patients. Group I (n=7) was administrated intermittent PTH after surgical treatment and group II (n=7) was treated only with surgery. We checked the time of initial callus formation, bridging callus formation, and bone union through periodic follow-up radiographs by a radiologist who did not know the patient's information.
RESULTS
The mean time to initial callus formation was 6 weeks for group I, compared with 6.7 weeks for group II. The mean time to bridging callus formation was 15.9 weeks for group I, compared with 23.0 weeks for group II. The mean time to bone union was 28.7 weeks for group I, compared with 41.9 weeks for group II. The difference in the cumulative detection rate (CDR) of the initial callus formation of group I and II was not statistically significant (p=0.793). However, the CDR of the bridging callus formation and bone union for group I were higher than those of group II (p=0.008, p=0.001, respectively).
CONCLUSION
The intermittent PTH administration after surgical treatment and maximum possible preservation of the periosteum in elderly patients accelerates fracture healing.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Bone Substitutes and the Advancement for Enhancing Bone Healing
Dong-Hyun Lee, Ji Wan Kim
J Korean Fract Soc. 2017;30(2):102-109. doi: 10.12671/jkfs.2017.30.2.102.Current Role and Application of Teriparatide in Fracture Healing of Osteoporotic Patients: A Systematic Review
Sang-Min Kim, Kyung-Chung Kang, Ji Wan Kim, Seung-Jae Lim, Myung Hoon Hahn
J Bone Metab. 2017;24(1):65-73. doi: 10.11005/jbm.2017.24.1.65.
Reference
-
1. Alkhiary YM, Gerstenfeld LC, Krall E, et al. Enhancement of experimental fracture-healing by systemic administration of recombinant human parathyroid hormone (PTH 1-34). J Bone Joint Surg Am. 2005. 87:731–741.
Article2. Aspenberg P, Genant HK, Johansson T, et al. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010. 25:404–414.
Article3. Bak B, Andreassen TT. The effect of aging on fracture healing in the rat. Calcif Tissue Int. 1989. 45:292–297.
Article4. Christian K, Thomas G. Robert WB, James DH, Charles MC, editors. Principles of internal fixation. Fractures in adults. 2005. 6th ed. Philadelphia: Lippincott-Raven;209–256.
Article5. Magnus KK, Karl JO, Per OJ. Robert WB, James DH, Charles MC, editors. Osteoporotic fractures. Fractures in adults. 2005. 6th ed. Philadelphia: Lippincott-Raven;614–641.
Article6. McCann RM, Colleary G, Geddis C, et al. Effect of osteoporosis on bone mineral density and fracture repair in a rat femoral fracture model. J Orthop Res. 2008. 26:384–393.
Article7. Naik AA, Xie C, Zuscik MJ, et al. Reduced COX-2 expression in aged mice is associated with impaired fracture healing. J Bone Miner Res. 2009. 24:251–264.
Article8. Peichl P, Holzer LA, Maier R, Holzer G. Parathyroid hormone 1-84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011. 93:1583–1587.
Article9. Skripitz R, Aspenberg P. Implant fixation enhanced by intermittent treatment with parathyroid hormone. J Bone Joint Surg Br. 2001. 83:437–440.
Article10. Watanabe Y, Matsushita T, Bhandari M, Zdero R, Schemitsch EH. Ultrasound for fracture healing: current evidence. J Orthop Trauma. 2010. 24:Suppl 1. S56–S61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intermittent Parathyroid Hormone Treatment for Stimulation of Callus Formation on Distal Femoral Fracture in Elderly Patients: Case Report
- Unusual Excessive Callus Formation in the Intertrochanteric Fracture Treated with Teriparatide
- Effect of Postoperative Parathyroid Hormone Administration on Osteoporotic Intertrochanteric Fractures of Females
- Erratum: Intermittent Parathyroid Hormone Treatment for Stimulation of Callus Formation in Elderly Patients
- Effects of Teriparatide Administration on Fracture Healing after Intramedullary Nailing in Atypical Femoral Fractures