J Korean Med Sci.
2013 Feb;28(2):320-327. 10.3346/jkms.2013.28.2.320.
Specific Activity Types at the Time of Event and Outcomes of Out-of-Hospital Cardiac Arrest: A Nationwide Observational Study
- Affiliations
-
- 1Department of Emergency Medicine and Cardiology, Seoul National University Hospital, Seoul, Korea.
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. shinsangdo@medimail.co.kr
- 3Department of Public Health, Seoul National University Graduate School of Public Health, Seoul, Korea.
- 4Department of Emergency Medicine, Korea University College of Medicine, Seoul, Korea.
- 5Department of Emergency Medicine, Seoul City Municipal Boramae Medical Center, Seoul National University, Seoul, Korea.
- KMID: 1429214
- DOI: http://doi.org/10.3346/jkms.2013.28.2.320
Abstract
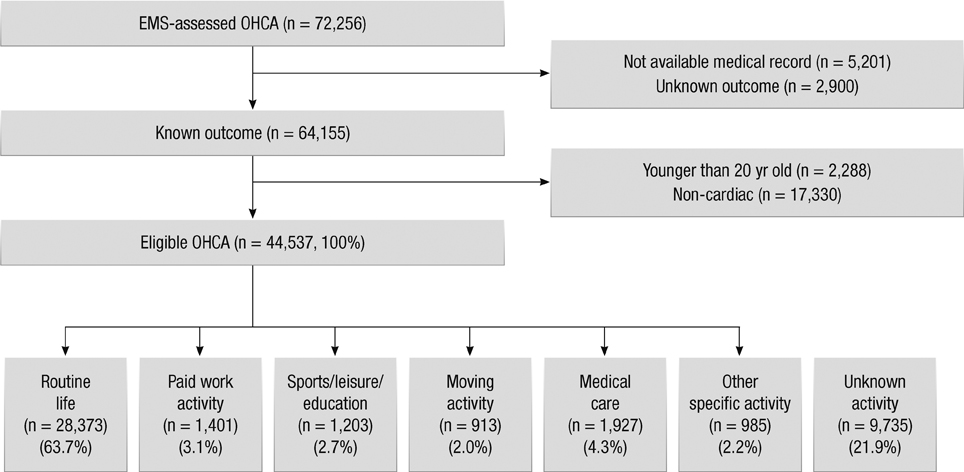
- This study aimed to describe the characteristics of out-of-hospital cardiac arrest (OHCA) according to specific activity types at the time of event and to determine the association between activities and outcomes according to activity type at the time of event occurrence of OHCA. A nationwide OHCA cohort database, compiled from January 2008 to December 2010 and consisting of hospital chart reviews and ambulance run sheet data, was used. Activity group was categorized as one of the following types: paid work activity (PWA), sports/leisure/education (SLE), routine life (RL), moving activity (MA), medical care (MC), other specific activity (OSA), and unknown activity. The main outcome was survival to discharge. Multivariate logistic analysis for outcomes was used adjusted for potential risk factors (reference = RL group). Of the 72,256 OHCAs, 44,537 cases were finally analyzed. The activities were RL (63.7%), PWA (3.1%), SLE (2.7%), MA (2.0%), MC (4.3%), OSA (2.2%), and unknown (21.9%). Survival to discharge rate for total patients was 3.5%. For survival to discharge, the adjusted odds ratios (95% confidence intervals) were 1.42 (1.06-1.90) in the SLE group and 1.62 (1.22-2.15) in PWA group compared with RL group. In conclusion, the SLE and PWA groups show higher survival to discharge rates than the routine life activity group.
Keyword
MeSH Terms
-
Activities of Daily Living
Adult
Aged
Aged, 80 and over
Ambulances
*Cardiopulmonary Resuscitation
Cohort Studies
Databases, Factual
Emergency Medical Services
Exercise
Female
Humans
Logistic Models
Male
Middle Aged
Odds Ratio
Out-of-Hospital Cardiac Arrest/classification/etiology/*mortality
Patient Discharge
Risk Factors
Survival Rate
Treatment Outcome
Work
Figure
Reference
-
1. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008. 300:1423–1431.2. Kim JH, Malhotra R, Chiampas G, d'Hemecourt P, Troyanos C, Cianca J, Smith RN, Wang TJ, Roberts WO, Thompson PD, et al. Cardiac arrest during long-distance running races. N Engl J Med. 2012. 366:130–140.3. Harmon KG, Drezner JA. Update on sideline and event preparation for management of sudden cardiac arrest in athletes. Curr Sports Med Rep. 2007. 6:170–176.4. Lotfi K, White L, Rea T, Cobb L, Copass M, Yin L, Becker L, Eisenberg M. Cardiac arrest in schools. Circulation. 2007. 116:1374–1379.5. Drezner JA, Rao AL, Heistand J, Bloomingdale MK, Harmon KG. Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009. 120:518–525.6. Mancini ME, Cazzell M, Kardong-Edgren S, Cason CL. Improving workplace safety training using a self-directed CPR-AED learning program. AAOHN J. 2009. 57:159–167.7. Ahn KO, Shin SD, Suh GJ, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest in Korea: A nationwide observational study. Resuscitation. 2010. 81:974–981.8. Ahn KO, Shin SD, Hwang SS, Oh J, Kawachi I, Kim YT, Kong KA, Hong SO. Association between deprivation status at community level and outcomes from out-of-hospital cardiac arrest: a nationwide observational study. Resuscitation. 2011. 82:270–276.9. Shin SD, Suh GJ, Ahn KO, Song KJ. Cardiopulmonary resuscitation outcome of out-of-hospital cardiac arrest in low-volume versus high-volume emergency departments: an observational study and propensity score matching analysis. Resuscitation. 2011. 82:32–39.10. World Health Organization. International Classification of External Causes of Injuries. accessed on 16 June 2012. Available at http://www.who.int/classifications/icd/adaptations/iceci/en/.11. Marijon E, Tafflet M, Celermajer DS, Dumas F, Perier MC, Mustafic H, Toussaint JF, Desnos M, Rieu M, Benameur N, et al. Sports-related sudden death in the general population. Circulation. 2011. 124:672–681.12. Holst AG, Winkel BG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, Svendsen JH, Haunsø S, Prescott E, Tfelt-Hansen J. Incidence and etiology of sports-related sudden cardiac death in Denmark: implications for preparticipation screening. Heart Rhythm. 2010. 7:1365–1371.13. Descatha A, Frederic M, Devere C, Dolveck F, Goddet S, Baer M, Chauvin M, Fletcher D, Templier F. Details of the initial management of cardiac arrest occurring in the workplace in a French urban area. Resuscitation. 2005. 65:301–307.14. Starr LM. American College of Occupational and Environmental Medicine. Automated external defibrillation in the occupational setting. J Occup Environ Med. 2002. 44:2–7.15. Bae H. Legal aspects of the application of the lay rescuer automatic external defibrillator (AED) program in South Korea. J Emerg Med. 2008. 34:299–303.16. Pun PH, Herzog CA, Middleton JP. Improving ascertainment of sudden cardiac death in patients with end stage renal disease. Clin J Am Soc Nephrol. 2012. 7:116–122.17. Pun PH, Lehrich RW, Honeycutt EF, Herzog CA, Middleton JP. Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics. Kidney Int. 2011. 79:218–227.18. Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, Macera CA, Castaneda-Sceppa C. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007. 39:1435–1445.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of Neurological Outcomes in Out-of-Hospital Cardiac Arrest Survivors Treated with Therapeutic Hypothermia
- Spatiotemporal Analysis of Out-ofHospital Cardiac Arrest Incidence and Survival Outcomes in Korea (2009–2021)
- Risk factors associated with inpatient cardiac arrest during emergency endotracheal intubation at general wards
- Interactive effect of multi-tier response and advanced airway management on clinical outcomes after out-of-hospital cardiac arrest: a nationwide population-based observational study
- Current Status of CPR in Korea