J Korean Med Sci.
2024 Mar;39(9):e86. 10.3346/jkms.2024.39.e86.
Spatiotemporal Analysis of Out-ofHospital Cardiac Arrest Incidence and Survival Outcomes in Korea (2009–2021)
- Affiliations
-
- 1Department of Public Health Sciences, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 2Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea
- 3Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2553335
- DOI: http://doi.org/10.3346/jkms.2024.39.e86
Abstract
- Background
Out-of-hospital cardiac arrest is a major public health concern in Korea. Identifying spatiotemporal patterns of out-of-hospital cardiac arrest incidence and survival outcomes is crucial for effective resource allocation and targeted interventions. Thus, this study aimed to investigate the spatiotemporal epidemiology of out-of-hospital cardiac arrest in Korea, with a focus on identifying high-risk areas and populations and examining factors associated with prehospital outcomes.
Methods
We conducted this population-based observational study using data from the Korean out-of-hospital cardiac arrest registry from January 2009 to December 2021. Using a Bayesian spatiotemporal model based on the Integrated Nested Laplace Approximation, we calculated the standardized incidence ratio and assessed the relative risk to compare the spatial and temporal distributions over time. The primary outcome was out-ofhospital cardiac arrest incidence, and the secondary outcomes included prehospital return of spontaneous circulation, survival to hospital admission and discharge, and good neurological outcomes.
Results
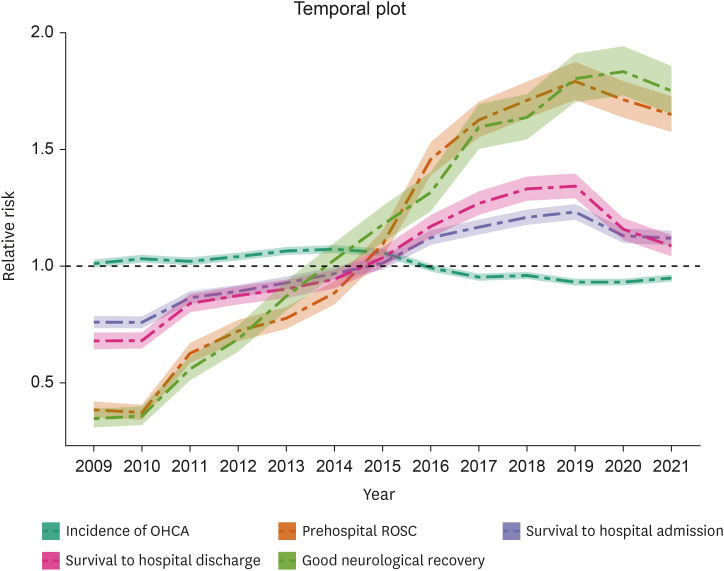
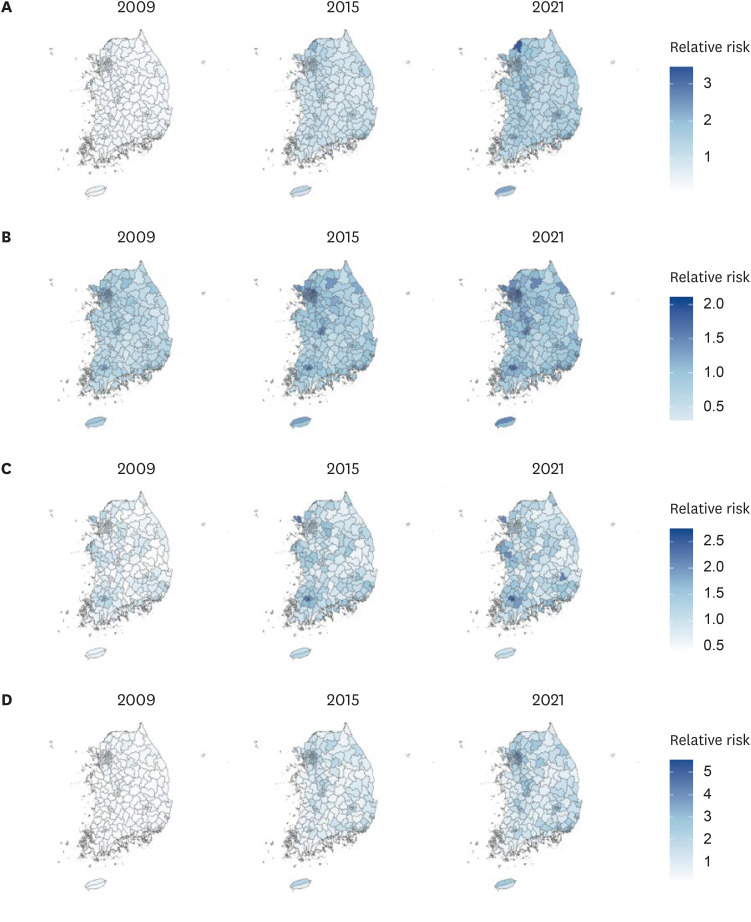
Although the number of cases increased over time, the spatiotemporal analysis exhibited a discernible temporal pattern in the standardized incidence ratio of out-ofhospital cardiac arrest with a gradual decline over time (1.07; 95% credible interval [CrI], 1.04–1.09 in 2009 vs. 1.00; 95% CrI, 0.98–1.03 in 2021). The district-specific risk ratios of survival outcomes were more favorable in the metropolitan and major metropolitan areas. In particular, the neurological outcomes were significantly improved from relative risk 0.35 (0.31–0.39) in 2009 to 1.75 (1.65–1.86) in 2021.
Conclusion
This study emphasized the significance of small-area analyses in identifying high-risk regions and populations using spatiotemporal analyses. These findings have implications for public health planning efforts to alleviate the burden of out-of-hospital cardiac arrest in Korea.
Figure
Reference
-
1. McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, et al. Out-of-hospital cardiac arrest surveillance—cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011; 60(8):1–19.2. Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018; 391(10124):970–979. PMID: 29536861.3. Mal PR, Sunnel P. Out-of-hospital cardiac arrest (OHCA): a critical healthcare problem. ECEC. 2019; 4:197–204.4. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010; 81(11):1479–1487. PMID: 20828914.5. Brooks SC, Clegg GR, Bray J, Deakin CD, Perkins GD, Ringh M, et al. Optimizing outcomes after out-of-hospital cardiac arrest with innovative approaches to public-access defibrillation: a scientific statement from the International Liaison Committee on Resuscitation. Circulation. 2022; 145(13):e776–e801. PMID: 35164535.6. Kim HS, Chun JH. Determinants on survival outcomes of sudden out-of-hospital cardiac arrest: a multilevel analysis. Korean J Emerg Med Serv. 2020; 24(2):7–26.7. Roh SY, Choi JI, Park SH, Kim YG, Shim J, Kim JS, et al. The 10-year trend of out-of-hospital cardiac arrests: a Korean nationwide population-based study. Korean Circ J. 2021; 51(10):866–874. PMID: 34595855.8. Korea Disease Control and Prevention Agency. Sudden cardiac arrest survey statistics report. Updated 2021. Accessed March 20, 2023. https://www.kdca.go.kr/injury/biz/injury/recsroom/statsSmMain.do;jsessionid=fmr-S-ZnRqrC9czcb5QeLbmEAW_TBn1HuNfYG6AI.injury10 .9. The Lancet. Out-of-hospital cardiac arrest: a unique medical emergency. Lancet. 2018; 391(10124):911. PMID: 29536841.10. Gowens P, Smith K, Clegg G, Williams B, Nehme Z. Global variation in the incidence and outcome of emergency medical services witnessed out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2022; 175:120–132. PMID: 35367317.11. Lerner EB, Rea TD, Bobrow BJ, Acker JE 3rd, Berg RA, Brooks SC, et al. Emergency medical service dispatch cardiopulmonary resuscitation prearrival instructions to improve survival from out-of-hospital cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2012; 125(4):648–655. PMID: 22230482.12. Rhee BY, Kim B, Lee YH. Effects of prehospital factors on survival of out-of-hospital cardiac arrest patients: age-dependent patterns. Int J Environ Res Public Health. 2020; 17(15):5481. PMID: 32751367.13. Chen CC, Chen CW, Ho CK, Liu IC, Lin BC, Chan TC. Spatial variation and resuscitation process affecting survival after out-of-hospital cardiac arrests (OHCA). PLoS One. 2015; 10(12):e0144882. PMID: 26659851.14. Doan TN, Wilson D, Rashford S, Ball S, Bosley E. Spatiotemporal variation in the risk of out-of-hospital cardiac arrests in Queensland, Australia. Resusc Plus. 2021; 8:100166. PMID: 34604821.15. Auricchio A, Peluso S, Caputo ML, Reinhold J, Benvenuti C, Burkart R, et al. Spatio-temporal prediction model of out-of-hospital cardiac arrest: Designation of medical priorities and estimation of human resources requirement. PLoS One. 2020; 15(8):e0238067. PMID: 32866165.16. Peluso S, Mira A, Rue H, Tierney NJ, Benvenuti C, Cianella R, et al. A Bayesian spatiotemporal statistical analysis of out-of-hospital cardiac arrests. Biom J. 2020; 62(4):1105–1119. PMID: 32011763.17. Wong PP, Low CT, Cai W, Leung KT, Lai PC. A spatiotemporal data mining study to identify high-risk neighborhoods for out-of-hospital cardiac arrest (OHCA) incidents. Sci Rep. 2022; 12(1):3509. PMID: 35241706.18. Lim SL, Smith K, Dyson K, Chan SP, Earnest A, Nair R, et al. Incidence and outcomes of out-of-hospital cardiac arrest in Singapore and Victoria: a collaborative study. J Am Heart Assoc. 2020; 9(21):e015981. PMID: 33094661.19. Root ED, Gonzales L, Persse DE, Hinchey PR, McNally B, Sasson C. A tale of two cities: the role of neighborhood socioeconomic status in spatial clustering of bystander CPR in Austin and Houston. Resuscitation. 2013; 84(6):752–759. PMID: 23318916.20. Sun CL, Karlsson L, Torp-Pedersen C, Morrison LJ, Folke F, Chan TC. Spatiotemporal AED optimization is generalizable. Resuscitation. 2018; 131:101–107. PMID: 30099121.21. Baumgarten MC, Röper J, Hahnenkamp K, Thies KC. Drones delivering automated external defibrillators-Integrating unmanned aerial systems into the chain of survival: a simulation study in rural Germany. Resuscitation. 2022; 172:139–145. PMID: 34971721.22. Kao JH, Chan TC, Lai F, Lin B, Sun W, Chang K, et al. Spatial analysis and data mining techniques for identifying risk factors of out-of-hospital cardiac arrest. Int J Inf Manage. 2017; 37(1):1528–1538.23. Fleming D, Owens A, Eckstein M, Sanko S. Spatiotemporal analysis of out-of-hospital cardiac arrest in the City of Los Angeles, 2011–2019. Resuscitation. 2021; 165:110–118. PMID: 34119555.24. Hwang SS, Ahn KO, Shin SD, Ro YS, Lee SY, Park JO, et al. Temporal trends in out-of-hospital cardiac arrest outcomes in men and women from 2008 to 2015: a national observational study. Am J Emerg Med. 2021; 41:174–178. PMID: 32029343.25. Ro YS, Hwang SS, Shin SD, Han D, Kang S, Song KJ, et al. Presumed regional incidence rate of out-of-hospital cardiac arrest in Korea. J Korean Med Sci. 2015; 30(10):1396–1404. PMID: 26425035.26. Korean Statistical Information Service. Summary of census population. Updated 2023. Accessed April 10, 2023. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPA001&conn_path=I2 .27. Song J, Ahn S, Kim J, Cho H, Moon S, Choi SH, et al. Sex-related disparities in the in-hospital management of patients with out-of-hospital cardiac arrest. Resuscitation. 2022; 173:47–55. PMID: 35151775.28. Choi DH, Ro YS, Kim KH, Park JH, Jeong J, Hong KJ, et al. The association between alcohol intake shortly before arrest and survival outcomes of out-of-hospital cardiac arrest. Resuscitation. 2022; 173:39–46. PMID: 35151774.29. Kwon JM, Jeon KH, Kim HM, Kim MJ, Lim S, Kim KH, et al. High incidence and mortality of out-of-hospital cardiac arrest on traditional holiday in South Korea. Korean Circ J. 2019; 49(10):945–956. PMID: 31165598.30. Choi Y, Park JH, Jeong J, Kim YJ, Song KJ, Shin SD. Extracorporeal cardiopulmonary resuscitation for adult out-of-hospital cardiac arrest patients: time-dependent propensity score-sequential matching analysis from a nationwide population-based registry. Crit Care. 2023; 27(1):87. PMID: 36879338.31. Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013; 84(5):547–557. PMID: 23313428.32. Becher H, Winkler V. Estimating the standardized incidence ratio (SIR) with incomplete follow-up data. BMC Med Res Methodol. 2017; 17(1):55. PMID: 28403811.33. Rue H, Martino S, Chopin N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Series B Stat Methodol. 2009; 71(2):319–392.34. Blangiardo M, Cameletti M, Baio G, Rue H. Spatial and spatio-temporal models with R-INLA. Spat Spatio-Temporal Epidemiol. 2013; 4:33–49.35. Naing NN. Easy way to learn standardization: direct and indirect methods. Malays J Med Sci. 2000; 7(1):10–15. PMID: 22844209.36. Moraga P. Small area disease risk estimation and visualization using R. R J. 2018; 10(1):495.37. Richardson S, Thomson A, Best N, Elliott P. Interpreting posterior relative risk estimates in disease-mapping studies. Environ Health Perspect. 2004; 112(9):1016–1025. PMID: 15198922.38. Rohleder S, Bozorgmehr K. Monitoring the spatiotemporal epidemiology of Covid-19 incidence and mortality: a small-area analysis in Germany. Spat Spatio-Temporal Epidemiol. 2021; 38:100433.39. Jaya IG, Folmer H. Bayesian spatiotemporal forecasting and mapping of COVID-19 risk with application to West Java Province, Indonesia. J Reg Sci. 2021; 61(4):849–881. PMID: 34230688.40. R Core Team. R: a language and environment for statistical computing. Updated 2022. Accessed March 20, 2023. https://www.R-project.org/ .41. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3(1):63–81. PMID: 20123673.42. Bielski K, Szarpak A, Jaguszewski MJ, Kopiec T, Smereka J, Gasecka A, et al. The influence of COVID-19 on out-hospital cardiac arrest survival outcomes: an updated systematic review and meta-analysis. J Clin Med. 2021; 10(23):5573. PMID: 34884289.43. Kim YS, Lee SH, Lim HJ, Hong WP. Impact of COVID-19 on out-of-hospital cardiac arrest in Korea. J Korean Med Sci. 2023; 38(12):e92. PMID: 36974401.44. Sasson C, Cudnik MT, Nassel A, Semple H, Magid DJ, Sayre M, et al. Identifying high-risk geographic areas for cardiac arrest using three methods for cluster analysis. Acad Emerg Med. 2012; 19(2):139–146. PMID: 22320364.45. Nassel AF, Root ED, Haukoos JS, McVaney K, Colwell C, Robinson J, et al. Multiple cluster analysis for the identification of high-risk census tracts for out-of-hospital cardiac arrest (OHCA) in Denver, Colorado. Resuscitation. 2014; 85(12):1667–1673. PMID: 25263511.46. Lym Y, Lym H, Kim K, Kim KJ. Spatiotemporal associations between local safety level index and COVID-19 infection risks across capital regions in South Korea. Int J Environ Res Public Health. 2022; 19(2):824. PMID: 35055645.47. Yum SG, Wei HH, Jang SH. Estimation of the non-exceedance probability of extreme storm surges in South Korea using tidal-gauge data. Nat Hazards Earth Syst Sci. 2021; 21(8):2611–2631.48. Lee M, An H, Jeon S, Kim S, Jung K, Park D. Development of an analytical probabilistic model to estimate runoff event volumes in South Korea. J Hydrol (Amst). 2022; 612:128129.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term Outcomes of the Combination of Vasopressin and Epinephrine versus Epinephrine Alone for Out-of-hospital Cardiac Arrest: A Prospective Observational Study
- Incidence and Outcome of Cardiac Arrest in Korea
- In-Hospital Cardiac Arrest: Patient Characteristics and Factors Influencing Survival and Neurologic Outcomes
- Comparison of CPR Outcomes between Autopulse TM and Manual Compression in Adult Out-of-hospital Cardiac Arrest
- Association between defoliant exposure and survival to discharge after out-of-hospital cardiac arrest