J Korean Neurosurg Soc.
2013 May;53(5):303-304. 10.3340/jkns.2013.53.5.303.
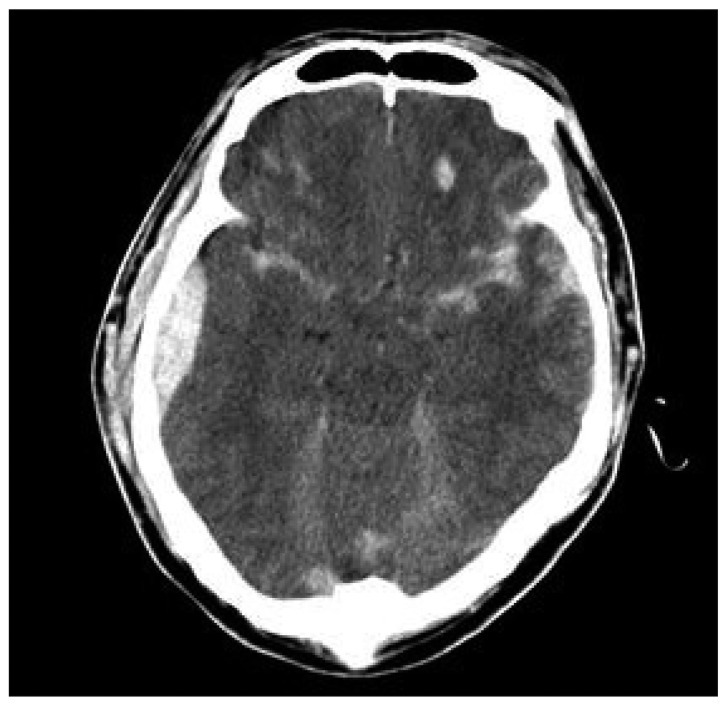
Fatal Rhabdomyolysis in a Patient with Head Injury
- Affiliations
-
- 1Department of Emergency Medicine, College of Medicine, Chosun University, Gwangju, Korea.
- 2Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 1426200
- DOI: http://doi.org/10.3340/jkns.2013.53.5.303
Abstract
- Rhabdomyolysis is a rare but potentially life-threatening disorder caused by the release of injured skeletal muscle components into the circulation. The authors report a case of severe head injury, in which a hyperosmolar state and continuous seizure complicated by severe rhabdomyolysis and acute renal failure evolved during the course of treatment resulted in a fatal outcome despite intensive supportive treatment. Our bitter experience suggests that rhabdomyolysis should be born in mind in patients with severe head injury who may develop hyperosmolar state and continuous seizure.
Keyword
MeSH Terms
Figure
Reference
-
1. Briggs TB, Smith RR. Exertional rhabdomyolysis associated with decerebrate posturing. Neurosurgery. 1986; 19:297–299. PMID: 3748364.
Article2. Chen CM, Chen JC, Kao MC. Severe rhabdomyolysis with good recovery in a patient with head injury : case report. Neurosurgery. 1997; 41:293–296. PMID: 9218322.
Article3. Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review : rhabdomyolysis -- an overview for clinicians. Crit Care. 2005; 9:158–169. PMID: 15774072.4. Jeon HJ, Cho BM, Oh SM, Park SH. Lumbosacral plexopathy, complicating rhabdomyolysis in a 57-year-old man, presented with sudden weakness in both legs. J Korean Neurosurg Soc. 2007; 42:481–483. PMID: 19096594.
Article5. Knochel JP, Carter NW. The role of muscle cell injury in the pathogenesis of acute renal failure after exercise. Kidney Int Suppl. 1976; 6:S58–S64. PMID: 135855.6. Larner AJ. Rhabdomyolysis associated with cranial diabetes insipidus. Postgrad Med J. 1992; 68:149. PMID: 1520370.
Article7. Owen CA, Mubarak SJ, Hargens AR, Rutherford L, Garetto LP, Akeson WH. Intramuscular pressures with limb compression clarification of the pathogenesis of the drug-induced muscle-compartment syndrome. N Engl J Med. 1979; 300:1169–1172. PMID: 431646.8. Poels PJ, Gabreels FJ. Rhabdomyolysis : a review of the literature. Clin Neurol Neurosurg. 1993; 95:175–192. PMID: 8242960.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal Rhabdomyolysis following Spine Surgery in a Morbidly Obese Patient: A Case Report
- Hyperkalemia in a patient with rhabdomyolysis and compartment syndrome: A case report
- A Case of Mushroom Poisoning with Russula subnigricans: Development of Rhabdomyolysis, Acute Kidney Injury, Cardiogenic Shock, and Death
- Rhabdomyolysis Induced Acute Kidney Injury in a Patient with Leptospirosis
- A Case of Rhabdomyolysis and Acute Renal Failure Associated with Salmonella Enteritidis