Is the Supraspinatus Muscle Atrophy Truly Irreversible after Surgical Repair of Rotator Cuff Tears?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Konkuk University Hospital, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Orthopaedic Surgery, Dongguk University Ilsan Hospital, Goyang, Korea.
- 4Department of Orthopaedic Surgery, Kyungpook National University Hospital, Daegu, Korea.
- 5Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 6Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. ohjh1@snu.ac.kr
- KMID: 1402327
- DOI: http://doi.org/10.4055/cios.2013.5.1.55
Abstract
- BACKGROUND
Atrophy of rotator cuff muscles has been considered an irreversible phenomenon. The purpose of this study is to evaluate whether atrophy is truly irreversible after rotator cuff repair.
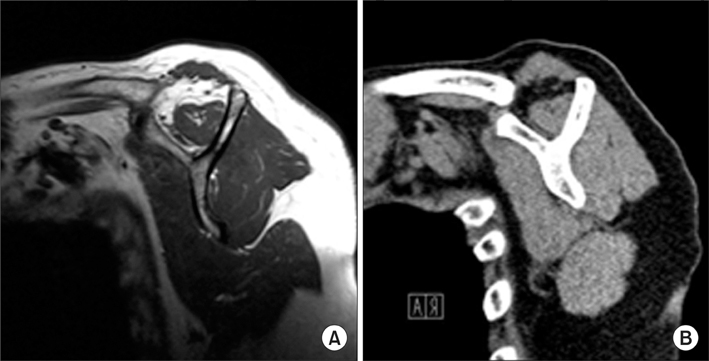
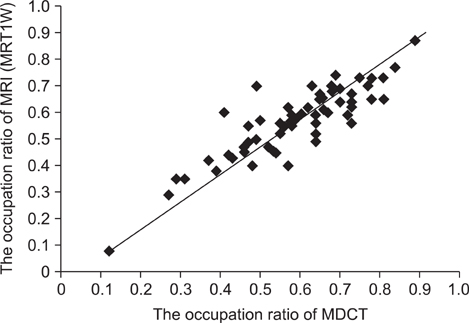
METHODS
We measured supraspinatus muscle atrophy of 191 patients with full-thickness rotator cuff tears on preoperative magnetic resonance imaging and postoperative multidetector computed tomography images, taken at least 1 year after operation. The occupation ratio was calculated using Photoshop CS3 software. We compared the change between pre- and postoperative occupation ratios after modifying the preoperative occupation ratio. In addition, possible relationship between various clinical factors and the change of atrophy, and between the change of atrophy and cuff integrity after surgical repair were evaluated.
RESULTS
The mean occupation ratio was significantly increased postoperatively from 0.44 +/- 0.17 to 0.52 +/- 0.17 (p < 0.001). Among 191 patients, 81 (42.4%) showed improvement of atrophy (more than a 10% increase in occupation ratio) and 33 (17.3%) worsening (more than a 10% decrease). Various clinical factors such as age tear size, or initial degree of atrophy did not affect the change of atrophy. However, the change of atrophy was related to repair integrity: cuff healing failure rate of 48.5% (16 of 33) in worsened atrophy; and 22.2% (18 of 81) in improved atrophy (p = 0.007).
CONCLUSIONS
The supraspinatus muscle atrophy as measured by occupation ratio could be improved postoperatively in case of successful cuff repair.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
The Accuracy of Sonoelastography in a Fatty Degeneration of Supraspinatus: A Comparison with Magnetic Resonance Images through Quantitative Assessment
Joong-Bae Seo, Jae-Sung Yoo, Jee-Won Ryu
J Korean Orthop Assoc. 2014;49(3):223-230. doi: 10.4055/jkoa.2014.49.3.223.A Follow-Up Study of Rotator Cuff Tear Using Magnetic Resonance Imaging
Jun-Sung Won, Woo-Seung Lee, Jae-Hong Park, Seung-Nam Ko, In-Wook Seo
J Korean Orthop Assoc. 2018;53(1):38-43. doi: 10.4055/jkoa.2018.53.1.38.Quantitative Measurement of Muscle Atrophy and Fat Infiltration of the Supraspinatus Muscle Using Ultrasonography After Arthroscopic Rotator Cuff Repair
Yong Ki Kim, Eun Seok Choi, Keon Tae Kim, Jung Ro Yoon, Sang Han Chae
Ann Rehabil Med. 2018;42(2):260-269. doi: 10.5535/arm.2018.42.2.260.
Reference
-
1. Bastard JP, Maachi M, Lagathu C, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006. 17(1):4–12.2. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994. (304):78–83.3. Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006. 88(3):472–479.4. Meyer DC, Hoppeler H, von Rechenberg B, Gerber C. A pathomechanical concept explains muscle loss and fatty muscular changes following surgical tendon release. J Orthop Res. 2004. 22(5):1004–1007.5. Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007. 35(5):719–728.6. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003. 12(6):550–554.7. Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010. 468(6):1498–1505.8. Mellado JM, Calmet J, Olona M, et al. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005. 184(5):1456–1463.9. Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000. 82(4):505–515.10. Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009. 25(1):30–39.11. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly: assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996. 67(3):264–268.12. Tae SK, Oh JH, Kim SH, Chung SW, Yang JY, Back YW. Evaluation of fatty degeneration of the supraspinatus muscle using a new measuring tool and its correlation between multidetector computed tomography and magnetic resonance imaging. Am J Sports Med. 2011. 39(3):599–606.13. Fuchs B, Gilbart MK, Hodler J, Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006. 88(2):309–316.14. Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am. 2007. 89(8):1770–1776.15. Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg. 2010. 19(1):14–20.16. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008. 190(4):1105–1111.17. Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007. 89(7):1533–1541.18. Bjorkenheim JM. Structure and function of the rabbit's supraspinatus muscle after resection of its tendon. Acta Orthop Scand. 1989. 60(4):461–463.19. Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000. 82(3):304–314.20. Meyer DC, Pirkl C, Pfirrmann CW, Zanetti M, Gerber C. Asymmetric atrophy of the supraspinatus muscle following tendon tear. J Orthop Res. 2005. 23(2):254–258.21. Nakagaki K, Ozaki J, Tomita Y, Tamai S. Fatty degeneration in the supraspinatus muscle after rotator cuff tear. J Shoulder Elbow Surg. 1996. 5(3):194–200.22. Rittweger J, Frost HM, Schiessl H, et al. Muscle atrophy and bone loss after 90 days' bed rest and the effects of flywheel resistive exercise and pamidronate: results from the LTBR study. Bone. 2005. 36(6):1019–1029.23. Tyml K, Mathieu-Costello O. Structural and functional changes in the microvasculature of disused skeletal muscle. Front Biosci. 2001. 6:D45–D52.24. Baar K, Nader G, Bodine S. Resistance exercise, muscle loading/unloading and the control of muscle mass. Essays Biochem. 2006. 42:61–74.25. Reynolds TH 4th, Bodine SC, Lawrence JC Jr. Control of Ser2448 phosphorylation in the mammalian target of rapamycin by insulin and skeletal muscle load. J Biol Chem. 2002. 277(20):17657–17662.26. Burridge K, Chrzanowska-Wodnicka M. Focal adhesions, contractility, and signaling. Annu Rev Cell Dev Biol. 1996. 12:463–518.27. Philippou A, Halapas A, Maridaki M, Koutsilieris M. Type I insulin-like growth factor receptor signaling in skeletal muscle regeneration and hypertrophy. J Musculoskelet Neuronal Interact. 2007. 7(3):208–218.28. Spangenburg EE, Booth FW. Leukemia inhibitory factor restores the hypertrophic response to increased loading in the LIF(-/-) mouse. Cytokine. 2006. 34(3-4):125–130.29. Gerber C, Meyer DC, Frey E, et al. Neer Award 2007: reversion of structural muscle changes caused by chronic rotator cuff tears using continuous musculotendinous traction. An experimental study in sheep. J Shoulder Elbow Surg. 2009. 18(2):163–171.30. Chung SW, Oh JH, Gong HS, Kim JY, Kim SH. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med. 2011. 39(10):2099–2107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MRI Follow-up Study After Arthroscopic Repair of Multiple Rotator Cuff Tendons
- Arthroscopic supraspinatus advancement for retracted rotator cuff tears: a technical note
- Surgical Options for Failed Rotator Cuff Repair, except Arthroplasty: Review of Current Methods
- Revisional Rotator Cuff Repair
- Intramuscular Lipoma of the Supraspinatus Muscle with Supraspinatus Tendon Partial Tear