Clin Orthop Surg.
2013 Mar;5(1):36-43. 10.4055/cios.2013.5.1.36.
Factors Correlated with the Reducibility of Varus Deformity in Knee Osteoarthritis: An Analysis Using Navigation Guided TKA
- Affiliations
-
- 1Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea. jgkim7437@gmail.com
- KMID: 1402324
- DOI: http://doi.org/10.4055/cios.2013.5.1.36
Abstract
- BACKGROUND
We hypothesized that a number of clinical and radiologic parameters could influence the reducibility of varus deformity in total knee arthroplasty. The aim of this study was to identify the factors correlated with reducibility of varus deformity and predict more accurately the amount of medial soft tissue release required in varus deformity total knee arthroplasty.
METHODS
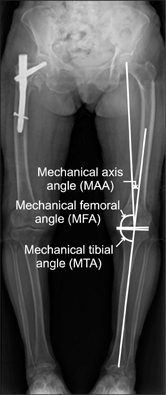
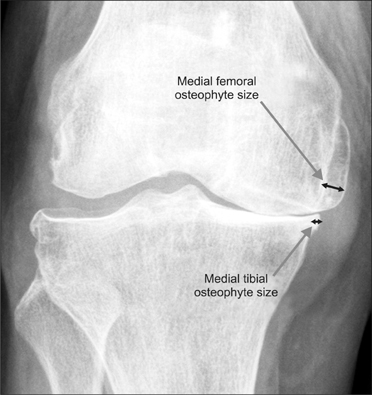
One hundred forty-three knees with preoperative varus alignment and medial osteoarthritis were included in this retrospective study. The total knee arthroplasties were performed using a navigation system (OrthoPilot) by single surgeon. To assess varus deformity, the authors measured preoperative mechanical axis angles and valgus stress angles. Mechanical tibial angles, mechanical femoral angles, femoral osteophyte sizes, and tibial osteophyte sizes were measured. The Ahlback grading scale was applied for radiologic parameters, and clinical parameters (age, body mass index, sex, duration of pain, and preoperative range of motion) were documented. Correlations between these factors and preoperative valgus stress angle were analyzed.
RESULTS
A negative correlation was found between preoperative mechanical axis angle and preoperative valgus stress angle (p < 0.01, r = -0.38), and a positive correlation was found between the preoperative mechanical tibial angle and preoperative valgus stress angle (p = 0.01, r = 0.19).
CONCLUSIONS
The present study shows that preoperative varus deformity and proximal tibial vara (measured by preoperative mechanical axis angle and mechanical tibial angle, respectively) are correlated with reducibility of varus deformity (measured by preoperative valgus stress angle), and clinical parameters (age, range of motion, duration of pain and body mass index) and other radiologic parameters (osteophyte size, severity of osteoarthritis and angulation of distal femoral joint surface) were not significantly correlated with reducibility of varus deformity.
Keyword
MeSH Terms
Figure
Reference
-
1. Verdonk PC, Pernin J, Pinaroli A, Ait Si Selmi T, Neyret P. Soft tissue balancing in varus total knee arthroplasty: an algorithmic approach. Knee Surg Sports Traumatol Arthrosc. 2009. 17(6):660–666.2. Ahlbäck S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh). 1968. Suppl 277. 7–72.3. Yagishita K, Muneta T, Ikeda H. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty. 2003. 18(3):313–320.4. Engh GA. The difficult knee: severe varus and valgus. Clin Orthop Relat Res. 2003. (416):58–63.5. Whiteside LA, Saeki K, Mihalko WM. Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000. (380):45–57.6. Engh GA, Ammeen D. Results of total knee arthroplasty with medial epicondylar osteotomy to correct varus deformity. Clin Orthop Relat Res. 1999. (367):141–148.7. Yasgur DJ, Scuderi GR, Insall JN. Scuderi GR, Tria AJ, editors. Medial release for fixed-varus deformity. Surgical techniques in total knee arthroplasty. 2002. New York: Springer-Verlag;189–196.8. Moon YW, Kim JG, Woo KJ, Lim SJ, Seo JG. Analysis of medial flexion gap after medial release for varus deformity by navigation-guided TKA. Orthopedics. 2011. 34(5):355.9. Noyes FR, Barber-Westin SD. Noyes FR, Barber-Westin SD, editors. Medial and posteromedial ligament injuries: diagnosis, operative techniques, and clinical outcomes. Noyes' knee disorders: surgery, rehabilitation, clinical outcomes. 2010. Philadelphia: Saunders Elsevier;661–691.10. Hernborg J, Nilsson BE. The relationship between osteophytes in the knee joint, osteoarthritis and aging. Acta Orthop Scand. 1973. 44(1):69–74.11. Boegard T, Jonsson K. Radiography in osteoarthritis of the knee. Skeletal Radiol. 1999. 28(11):605–615.12. Saragaglia D, Chaussard C, Rubens-Duval B. Navigation as a predictor of soft tissue release during 90 cases of computer-assisted total knee arthroplasty. Orthopedics. 2006. 29:10 Suppl. S137–S138.13. Saragaglia D, Picard F. Stiehl JB, Konermann WH, Haaker RG, editors. Computer assisted implantation of total knee endoprosthesis with no preoperative imaging: the kinematic model. Navigation and robotics in total joint and spine surgery. 2004. New York: Springer-Verlag;226–233.14. Krackow KA, Mihalko WM. The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft-tissue balancing in total knee arthroplasty. Am J Knee Surg. 1999. 12(4):222–228.15. Mullaji A, Sharma A, Marawar S, Kanna R. Quantification of effect of sequential posteromedial release on flexion and extension gaps: a computer-assisted study in cadaveric knees. J Arthroplasty. 2009. 24(5):795–805.16. Luring C, Hufner T, Perlick L, Bathis H, Krettek C, Grifka J. The effectiveness of sequential medial soft tissue release on coronal alignment in total knee arthroplasty: using a computer navigation model. J Arthroplasty. 2006. 21(3):428–434.17. Williams JM, Brandt KD. Exercise increases osteophyte formation and diminishes fibrillation following chemically induced articular cartilage injury. J Anat. 1984. 139(Pt 4):599–611.18. Gelse K, Soder S, Eger W, Diemtar T, Aigner T. Osteophyte development--molecular characterization of differentiation stages. Osteoarthritis Cartilage. 2003. 11(2):141–148.19. Hashimoto S, Creighton-Achermann L, Takahashi K, Amiel D, Coutts RD, Lotz M. Development and regulation of osteophyte formation during experimental osteoarthritis. Osteoarthritis Cartilage. 2002. 10(3):180–187.20. Pottenger LA, Phillips FM, Draganich LF. The effect of marginal osteophytes on reduction of varus-valgus instability in osteoarthritic knees. Arthritis Rheum. 1990. 33(6):853–858.21. Cooke TD, Siu D, Fisher B. Noble J, Galasko CS, editors. The use of standardized radiographs to identify the deformities associated with osteoarthritis. Recent developments in orthopedic surgery. 1987. Manchester: Manchester University Press;264–273.22. Kolstad K, Sahlstedt B, Wigren A. Extension deficit and lateral instability in degenerative disease of the knee. Acta Orthop Scand. 1980. 51(4):667–672.23. Hayashi K. Biomechanical studies of the remodeling of knee joint tendons and ligaments. J Biomech. 1996. 29(6):707–716.24. Binkley JM, Peat M. The effects of immobilization on the ultrastructure and mechanical properties of the medial collateral ligament of rats. Clin Orthop Relat Res. 1986. (203):301–308.25. Cooke TD, Pichora D, Siu D, Scudamore RA, Bryant JT. Surgical implications of varus deformity of the knee with obliquity of joint surfaces. J Bone Joint Surg Br. 1989. 71(4):560–565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Radiologic Measurements of Total Knee Replacement using Computer-assisted Navigation System and Conventional System in Varus Deformity of the Knee
- Relationship between Lateral Femoral Bowing and Varus Knee Deformity Based on Two-Dimensional Assessment of Side-to-Side Differences
- Navigation-Assisted Total Knee Arthroplasty for Patients with Extra-Articular Deformity
- Preoperative Varus-Valgus Stress Angle Difference Is Valuable for Predicting the Extent of Medial Release in Varus Deformity during Total Knee Arthroplasty
- Effects of Femoral Lateral Bowing on Coronal Alignment and Component Position after Total Knee Arthroplasty: A Comparison of Conventional and Navigation-Assisted Surgery