Korean J Radiol.
2012 Dec;13(6):795-802. 10.3348/kjr.2012.13.6.795.
Percutaneous Biliary Drainage Using Open Cell Stents for Malignant Biliary Hilar Obstruction
- Affiliations
-
- 1Department of Radiology, Ajou University School of Medicine, Suwon 443-380, Korea. jaeikbae@naver.com
- KMID: 1397511
- DOI: http://doi.org/10.3348/kjr.2012.13.6.795
Abstract
OBJECTIVE
To evaluate the feasibility, safety and the effectiveness of the complex assembly of open cell nitinol stents for biliary hilar malignancy.
MATERIALS AND METHODS
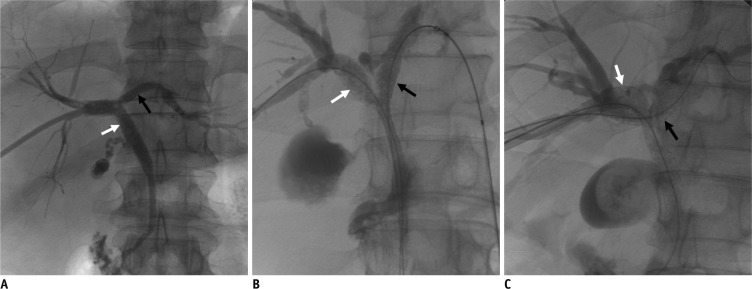
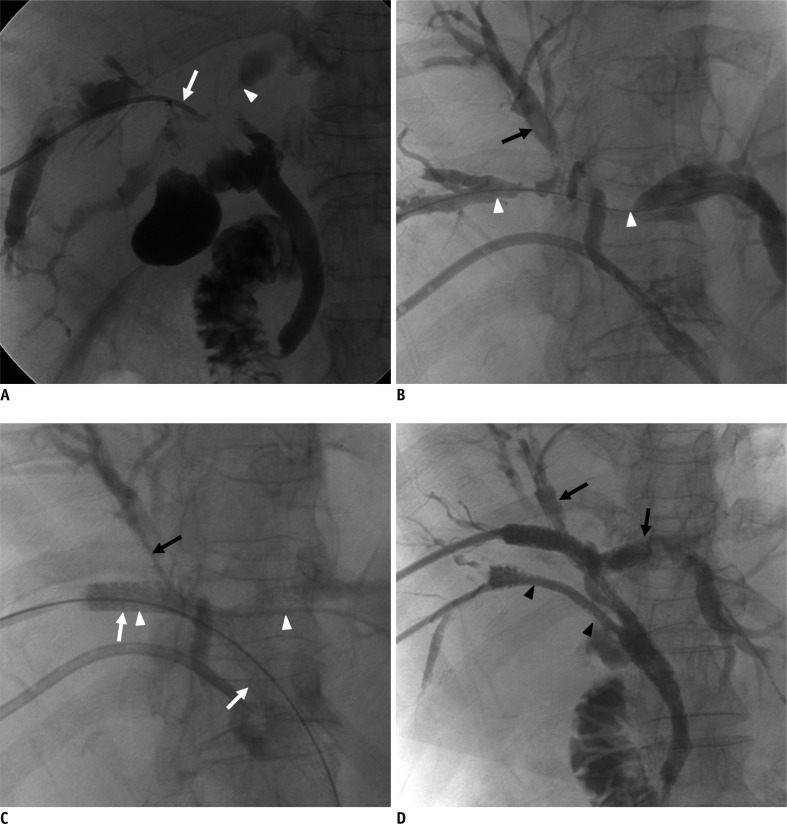
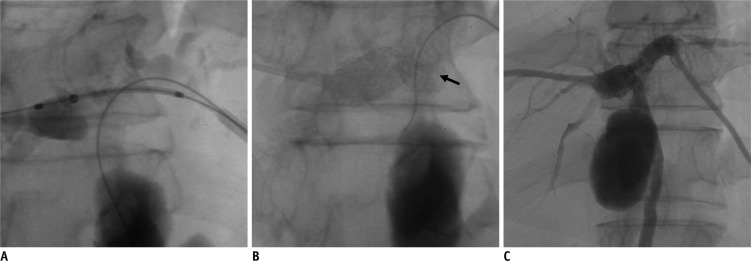
During the 10 month period between January and October 2007, 26 consecutive patients with malignant biliary hilar obstruction underwent percutaneous insertion of open cell design nitinol stents. Four types of stent placement methods were used according to the patients' ductal anatomy of the hilum. We evaluated the technical feasibility of stent placement, complications, patient survival, and the duration of stent patency.
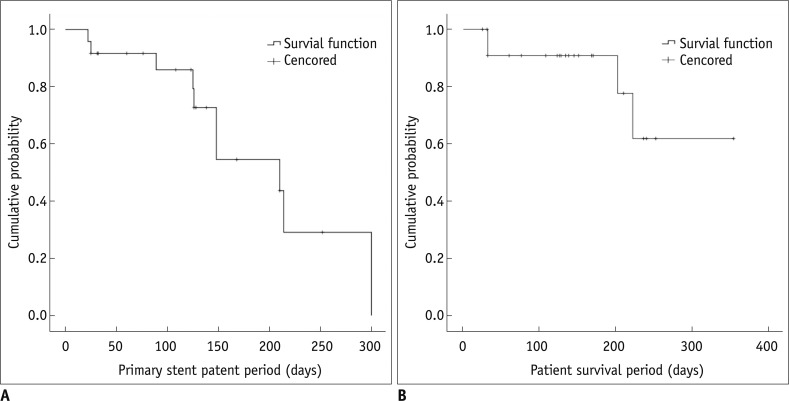
RESULTS
Bilobar biliary stent placement was conducted in 26 patients with malignant biliary obstruction-T (n = 9), Y (n = 7), crisscross (n = 6) and multiple intersecting types (n = 4). Primary technical success was obtained in 24 of 26 (93%) patients. The crushing of the 1st stent during insertion of the 2nd stent occurred in two cases. Major complications occurred in 2 of 26 patients (7.7%). One case of active bleeding from hepatic segmental artery and one case of sepsis after procedure occurred. Clinical success was achieved in 21 of 24 (87.5%) patients, who were followed for a mean of 141.5 days (range 25-354 days). The mean primary stent patency period was 191.8 days and the mean patient survival period was 299 days.
CONCLUSION
Applying an open cell stent in the biliary system is feasible, and can be effective, especially in multiple intersecting stent insertions in the hepatic hilum.
MeSH Terms
Figure
Reference
-
1. Nordback IH, Pitt HA, Coleman J, Venbrux AC, Dooley WC, Yeu NN, et al. Unresectable hilar cholangiocarcinoma: percutaneous versus operative palliation. Surgery. 1994; 115:597–603. PMID: 7513906.2. LaBerge JM, Doherty M, Gordon RL, Ring EJ. Hilar malignancy: treatment with an expandable metallic transhepatic biliary stent. Radiology. 1990; 177:793–797. PMID: 2173842.
Article3. Kim CW, Park AW, Won JW, Kim S, Lee JW, Lee SH. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol. 2004; 15:713–717. PMID: 15231885.
Article4. Inal M, Akgül E, Aksungur E, Seydaoğlu G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol. 2003; 14:1409–1416. PMID: 14605106.
Article5. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553. PMID: 11323577.
Article6. Cowling MG, Adam AN. Internal stenting in malignant biliary obstruction. World J Surg. 2001; 25:355–359. discussion 359-361. PMID: 11343193.7. Rerknimitr R, Kladcharoen N, Mahachai V, Kullavanijaya P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol. 2004; 38:518–523. PMID: 15220688.
Article8. Choi KH, Cho YK, An JK, Woo JJ, Kim HS, Choi YS. Acute obstructive cholangitis after transarterial chemoembolization: the effect of percutaneous transhepatic removal of tumor fragment. Korean J Radiol. 2009; 10:197–201. PMID: 19270868.
Article9. Han YM, Kwak HS, Jin GY, Lee SO, Chung GH. Treatment of malignant biliary obstruction with a PTFE-covered self-expandable nitinol stent. Korean J Radiol. 2007; 8:410–417. PMID: 17923784.
Article10. Kim JH. Clinical feasibility and usefulness of CT fluoroscopy-guided percutaneous transhepatic biliary drainage in emergency patients with acute obstructive cholangitis. Korean J Radiol. 2009; 10:144–149. PMID: 19270860.
Article11. Lee JH, Kang DH, Kim JY, Lee SM, Kim do H, Park CW, et al. Endoscopic bilateral metal stent placement for advanced hilar cholangiocarcinoma: a pilot study of a newly designed Y stent. Gastrointest Endosc. 2007; 66:364–369. PMID: 17643714.
Article12. Topazian M. Toward a better biliary confluence stent. Gastrointest Endosc. 2007; 66:369–371. PMID: 17643715.
Article13. Duda SH, Wiskirchen J, Tepe G, Bitzer M, Kaulich TW, Stoeckel D, et al. Physical properties of endovascular stents: an experimental comparison. J Vasc Interv Radiol. 2000; 11:645–654. PMID: 10834499.
Article14. Sobolevsky SA, Rakin D, Janne d'Othee B, Lang EV. Complex stent assemblies: feasibility of stent-through-stent deployment. Cardiovasular and Interventional Society of Europe e-poster: P100 September 2006.15. Rutledge JM, Grifka RG, Bryant LL, Mullins CE, Vincent JA. Balloon dilation and stent implant through the side of a previously placed intravascular stent: a new option for the interventionalist. Catheter Cardiovasc Interv. 2002; 56:387–393. PMID: 12112895.
Article16. Pierce DS, Rosero EB, Modrall JG, Adams-Huet B, Valentine RJ, Clagett GP, et al. Open-cell versus closed-cell stent design differences in blood flow velocities after carotid stenting. J Vasc Surg. 2009; 49:602–606. discussion 606. PMID: 19268763.
Article17. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202. PMID: 14514818.
Article18. Bae JI, Park AW, Choi SJ, Kim HP, Lee SJ, Park YM, et al. Crisscross-configured dual stent placement for trisectoral drainage in patients with advanced biliary hilar malignancies. J Vasc Interv Radiol. 2008; 19:1614–1619. PMID: 18823794.
Article19. Dumas R, Demuth N, Buckley M, Peten EP, Manos T, Demarquay JF, et al. Endoscopic bilateral metal stent placement for malignant hilar stenoses: identification of optimal technique. Gastrointest Endosc. 2000; 51:334–338. PMID: 10699784.
Article20. Kim JY, Kang DH, Kim HW, Choi CW, Kim ID, Hwang JH, et al. Usefulness of slimmer and open-cell-design stents for endoscopic bilateral stenting and endoscopic revision in patients with hilar cholangiocarcinoma (with video). Gastrointest Endosc. 2009; 70:1109–1115. PMID: 19647244.
Article21. Müller-Hülsbeck S, Schäfer PJ, Charalambous N, Schaffner SR, Heller M, Jahnke T. Comparison of carotid stents: an in-vitro experiment focusing on stent design. J Endovasc Ther. 2009; 16:168–177. PMID: 19456191.
Article22. Park do H, Lee SS, Moon JH, Choi HJ, Cha SW, Kim JH, et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: multicenter prospective feasibility study (with videos). Gastrointest Endosc. 2009; 69:1357–1360. PMID: 19481654.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Technical Tips and Issues of Biliary Stenting, Focusing on Malignant Hilar Obstruction
- Endoscopic Ultrasound-Guided Biliary Drainage for Unresectable Hilar Malignant Biliary Obstruction
- Multiple metallic stents placement for malignant hilar biliary obstruction: Perspective of a radiologist
- Comparison of Long-term Complication of Malignant Biliary Obstruction after Percutaneous Transhepatic Biliary Drainage Versus Metallic Biliary Drainage