Korean J Gastroenterol.
2012 Apr;59(4):313-316. 10.4166/kjg.2012.59.4.313.
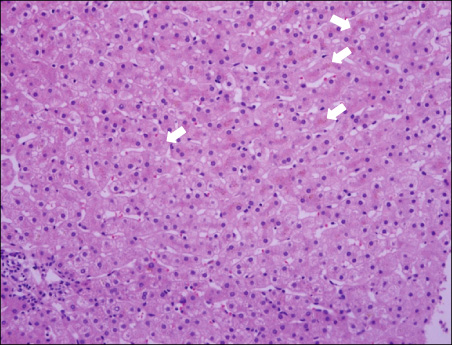
A Case of Sustained Cholestasis Caused by Acute A Viral Hepatitis in Dubin-Johnson Syndrome
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. drkimmy@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 1364836
- DOI: http://doi.org/10.4166/kjg.2012.59.4.313
Abstract
- Dubin-Johnson syndrome is a rare clinical entity. It shows intermittent symptoms such as chronic or intermittent jaundice, abdominal pain, weakness, nausea, vomiting, anorexia and diarrhea. Symptoms are precipitated or aggravated by pregnancy, alcoholism, surgical procedures and intercurrent disease. Chronic idiopathic jaundice is typical of Dubin-Johnson syndrome and its prognosis is good. We describe a case of prolonged cholestasis for more than 10 months caused by acute A viral hepatitis in a patient with Dubin-Johnson syndrome. It is a first report of cholestasis complicated by acute A viral hepatitis in a patient with Dubin-Johnson syndrome.
MeSH Terms
Figure
Reference
-
1. Dubin IN, Johnson FB. Chronic idiopathic jaundice with unidentified pigment in liver cells; a new clinicopathologic entity with a report of 12 cases. Medicine (Baltimore). 1954. 33:155–197.2. Butt HR, Anderson VE, Foulk WT, Baggenstoss AH, Schoenfield LJ, Dickson ER. Studies of chronic idiopathic jaundice (Dubin-Johnson syndrome). II. Evaluation of a large family with the trait. Gastroenterology. 1966. 51:619–630.3. Shani M, Seligsohn U, Gilon E, Sheba C, Adam A. Dubin-Johnson syndrome in Israel. I. Clinical, laboratory, and genetic aspects of 101 cases. Q J Med. 1970. 39:549–567.4. Toh S, Wada M, Uchiumi T, et al. Genomic structure of the canalicular multispecific organic anion-transporter gene (MRP2/cMOAT) and mutations in the ATP-binding-cassette region in Dubin-Johnson syndrome. Am J Hum Genet. 1999. 64:739–746.5. Swartz HM, Sarna T, Varma RR. On the natural and excretion of the hepatic pigment in the Dubin-Johnson syndrome. Gastroenterology. 1979. 76:958–964.6. Novikoff AB, Essner E, Quintana N. Golgi Apparatus and Lysosomes. Fed Proc. 1964. 23:1010–1022.7. Beker S, Read AE. Familial DubinJohnson syndrome. Gastroenterology. 1958. 35:387–389.8. Hahn SS, Hahn YC, Hahn YS, Choi KW, Min BC, Kim OJ. A case of Dubin-Johnson syndrome. Taehan Uihak Hyophoe Chi. 1963. 6:609–614.9. Berk PD. Bilirubin metabolism and the hereditary hyperbilirubinemias. Semin Liver Dis. 1994. 14:321–322.10. Cohen L, Lewis C, Arias IM. Pregnancy, oral contraceptives, and chronic familial jaundice with predominantly conjugated hyperbilirubinemia (Dubin-Johnson syndrome). Gastroenterology. 1972. 62:1182–1190.11. Koskelo P, Toivonen I, Adlercreutz H. Urinary coproporphyrin isomer distribution in the Dubin-Johnson syndrome. Clin Chem. 1967. 13:1006–1009.12. Koff RS. Hepatitis A. Lancet. 1998. 351:1643–1649.13. Ono S, Chida K, Takasu T. Guillain-Barré syndrome following fulminant viral hepatitis A. Intern Med. 1994. 33:799–801.14. Mourani S, Dobbs SM, Genta RM, Tandon AK, Yoffe B. Hepatitis A virus-associated cholecystitis. Ann Intern Med. 1994. 120:398–400.15. Inman RD, Hodge M, Johnston ME, Wright J, Heathcote J. Arthritis, vasculitis, and cryoglobulinemia associated with relapsing hepatitis A virus infection. Ann Intern Med. 1986. 105:700–703.16. Gordon SC, Reddy KR, Schiff L, Schiff ER. Prolonged intrahepatic cholestasis secondary to acute hepatitis A. Ann Intern Med. 1984. 101:635–637.17. Sciot R, Van Damme B, Desmet VJ. Cholestatic features in hepatitis A. J Hepatol. 1986. 3:172–181.18. Schiff ER. Atypical clinical manifestations of hepatitis A. Vaccine. 1992. 10:Suppl 1. S18–S20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Dubin-Johnson Syndrome
- A case of Dubin-Johnson syndrome with a pigmented neurofibroma
- Melanosis coli--histochemical and immunohistochemical comparison of the pigments of melanosis coli and Dubin-Johnson syndrome
- A Case of Stevens-Johnson Syndrome Plus Vanishing Bile Duct Syndrome Associated with Ibuprofen Use
- Stevens-Johnson Syndrome Caused by Dapsone