J Korean Rheum Assoc.
2008 Mar;15(1):76-80. 10.4078/jkra.2008.15.1.76.
Lobular Panniculitis in a Patient with Dermatomyositis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, The Hospital for Rheumatic Diseases, Hanyang University College of Medicine, Seoul, Korea. junjb@hanyang.ac.kr
- 2Department of Dermatology, Hanyang University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 1324513
- DOI: http://doi.org/10.4078/jkra.2008.15.1.76
Abstract
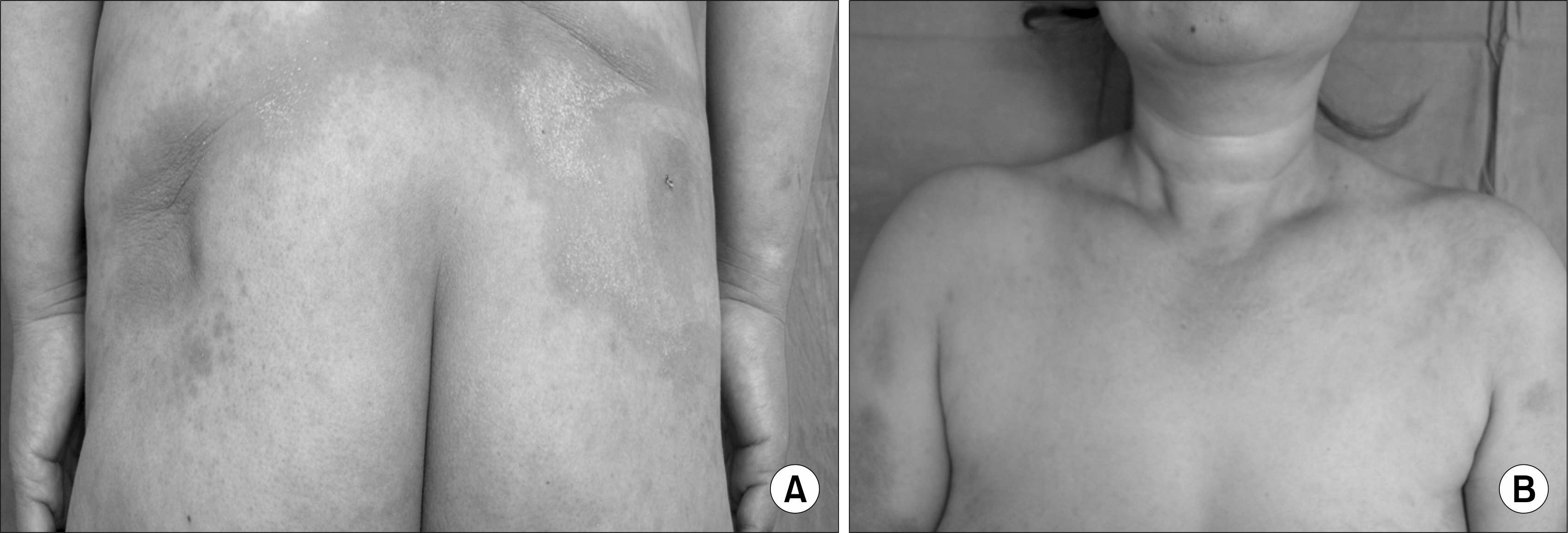
- Panniculitis is an inflammation within adipose tissue and most commonly affects the subcutaneous fat. Frequently, the panniculitis is associated with certain drugs and systemic diseases, such as various rheumatologic diseases, idiopathic Weber-Christian disease, infection and malignancy. Panniculitis in dermatomyositis (DM) is most commonly an incidental histopathologic finding that less commonly manifests a clinical component. We report the case of a woman with DM who presented with panniculitis as a clinical finding. A 51-year-old woman was admitted to our hospital with diffuse nodular, indurated, painful erythematous plaques on buttocks, back and chest. 18-months ago, she had been diagnosed DM at our hospital. Her medication on admission was azathioprine. High-dose glucocorticoid was prescribed after the diagnosis of lobular panniculitis confirmed by skin biopsy. After then, the patient was getting better and discharged with the medication tapered.
Keyword
Figure
Cited by 1 articles
-
Pancreatic Panniculitis in Patients with Chronic Pancreatitis: Case Report and Review of Literature
Eui Joong Kim, Min Su Chu, Ki Chang Sohn, Dong Ho Cho, Ga Hye Na, Haak Cheoul Kim, Eun Young Cho
Korean J Gastroenterol. 2017;69(1):83-86. doi: 10.4166/kjg.2017.69.1.83.
Reference
-
References
1. Eberhard BA, Ilowite NT. Panniculitis and lipodystrophy. Curr Opin Rheumatol. 2002; 14:566–70.
Article2. Ter Poorten MC, Thiers BH. Panniculitis. Dermatol Clin. 2002; 20:421–33.
Article3. Diaz Cascajo C, Borghi S, Weyers W. Panniculitis: definition of terms and diagnostic strategy. Am J Dermatopathol. 2000; 22:530–49.4. Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000; 39:141–4.
Article5. Solans R, Cortes J, Selva A, Garcia-Patos V, Jimenez FJ, Pascual C, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002; 46:S148–50.
Article6. Ghali FE, Reed AM, Groben PA, McCauliffe DP. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999; 16:270–2.7. Janis JF, Winkelmann RK. Histopathology of the skin in dermatomyositis. A histopathologic study of 55 cases. Arch Dermatol. 1968; 97:640–50.
Article8. Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995; 33:305–7.
Article9. Molnar K, Kemeny L, Korom I, Dobozy A. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998; 139:161–3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Lobular Panniculitis in Dermatomyositis Patient
- Dermatomyositis First Presenting as Panniculitis
- A Case of Factitial Panniculitis
- A Case of Atypical Lymphocytic Lobular Panniculitis
- Successful Treatment with Methotrexate and Azathioprine of Panniculitis in a Patient with Dermatomyositis: Case Report and Review of the Literature