Korean J Radiol.
2007 Apr;8(2):156-163. 10.3348/kjr.2007.8.2.156.
The Use of Magnetic Resonance Imaging to Predict the Clinical Outcome of Non-Surgical Treatment for Lumbar Interverterbal Disc Herniation
- Affiliations
-
- 1Department of Radiology, GangNeung Asan Hospital, University of Ulsan College of Medicine, GangNeung, Korea. songjs@kd.ac.kr
- 2Department of Preventive Medicine, University of Kwandong College of Medicine, GangNeung, Korea.
- 3Department of Orthopedic Surgery, GangNeung Asan Hospital, University of Ulsan College of Medicine, GangNeung, Korea.
- 4Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1126839
- DOI: http://doi.org/10.3348/kjr.2007.8.2.156
Abstract
OBJECTIVE
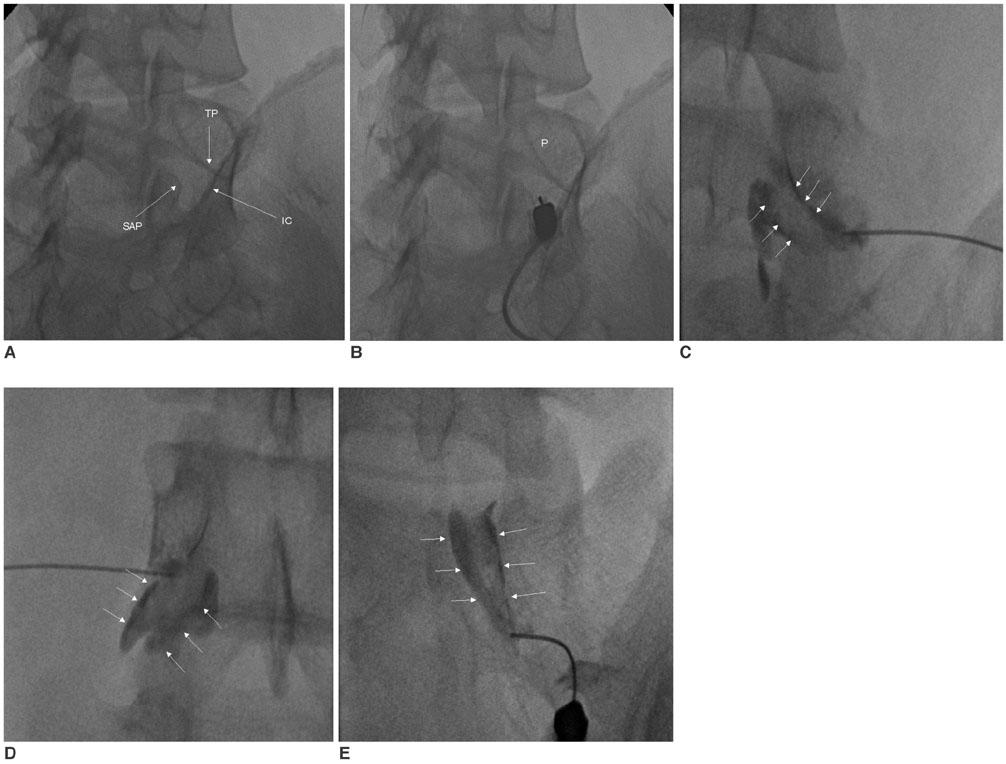
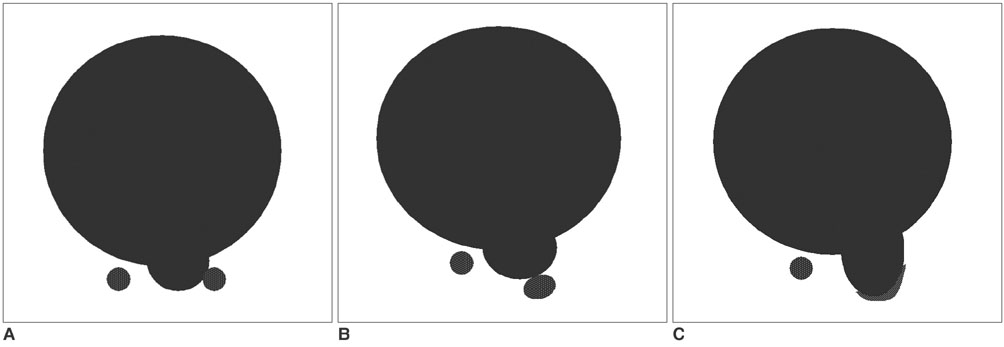
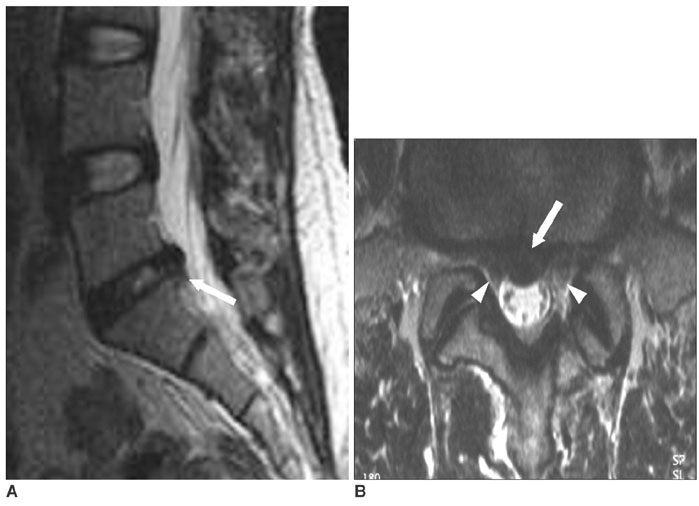
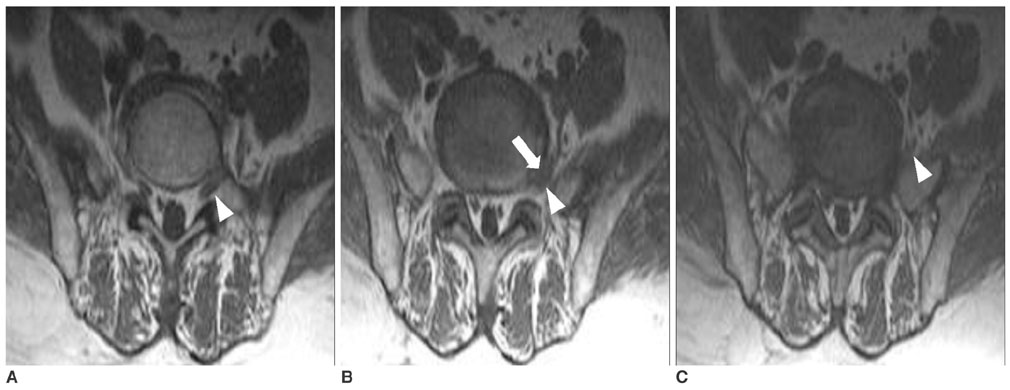
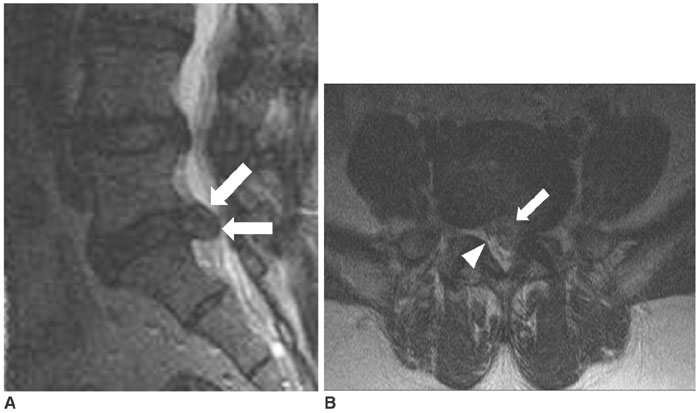
We wanted to investigate the relationship between the magnetic resonance (MR) findings and the clinical outcome after treatment with non-surgical transforaminal epidural steroid injections (ESI) for lumbar herniated intervertebral disc (HIVD) patients. MATERIALS AND METHODS: Transforaminal ESI were performed in 91 patients (50 males and 41 females, age range: 13-78 yrs) because of lumbosacral HIVD from March 2001 to August 2002. Sixty eight patients whose MRIs and clinical follow-ups were available were included in this study. The medical charts were retrospectively reviewed and the patients were divided into two groups; the successful (responders, n = 41) and unsatisfactory (non-responders, n = 27) outcome groups. A successful outcome required a patient satisfaction score greater than two and a pain reduction score greater than 50%. The MR findings were retrospectively analyzed and compared between the two groups with regard to the type (protrusion, extrusion or sequestration), hydration (the T2 signal intensity), location (central, right/left central, subarticular, foraminal or extraforaminal), and size (volume) of the HIVD, the grade of nerve root compression (grade 1 abutment, 2 displacement and 3 entrapment), and an association with spinal stenosis. RESULTS: There was no significant difference between the responders and non-responders in terms of the type, hydration and size of the HIVD, or an association with spinal stenosis (p > 0.05). However, the location of the HIVD and the grade of nerve root compression were different between the two groups (p < 0.05). CONCLUSION: MRI could play an important role in predicting the clinical outcome of non-surgical transforaminal ESI treatment for patients with lumbar HIVD.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effectiveness of Selective Nerve Root Block on the Need for Surgical Treatment of Lumbar Disc Herniation
Dae Moo Shim, Jin Young Park, Jung Hwan Yang, Byong San Choi
J Korean Orthop Assoc. 2008;43(4):413-419. doi: 10.4055/jkoa.2008.43.4.413.
Reference
-
1. Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica with associated disc pathology: a prospective study with clinical and independent radiologic follow-up. Spine. 1992. 17:1205–1212.2. Colonna PC, Fredienburg Z. The disc syndrome. J Bone Joint Surg (Am). 1949. 31:614–618.3. Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997. 336:1634–1640.4. White AH, Derby R, Wynne G. Epidural injections in the diagnosis and treatment of low-back pain. Spine. 1980. 5:78–86.5. Koes BW, Scholten RJ, Mens JM, Bouter LM. Efficacy of epidural steroid injections for low-back pain and sciatica; a systematic review of randomized clinical trials. Pain. 1995. 63:279–288.6. Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an out come study. Arch Phys Med Rehabil. 1998. 79:1362–1366.7. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002. 27:11–16.8. Simotas AC. Nonoperative treatment for lumbar spinal stenosis. Clin Orthop Relat Res. 2001. 384:153–161.9. Papagelopoulos PJ, Petrou HG, Triantafyllidis PG, Vlamis JA, Psomas-Pasalis M, Korres DS, et al. Treatment of lumbosacral radicular pain with epidural steroid injections. Orthopedics. 2001. 24:145–149.10. Viton JM, Peretti-Viton P, Rubino T, Delarque A, Salamon N. Short-term assessment of periradicular corticosteroid injections in lumbar radiculopathy associated with disc pathology. Neuroradiology. 1998. 40:59–62.11. Ahn SH, Ahn MW, Byun WM. Effect of the transligamentous extension of lumbar disc herniations on their regression and the clinical outcome of sciatica. Spine. 2000. 25:475–480.12. Matsubara Y, Kato F, Minatsu K, Nakamura S, Nitta H. Serial changes on MRI in lumbar disc herniations treated conservatively. Neuroradiology. 1995. 37:378–383.13. Gallucci M, Bozzao A, Orlandi B, Manetta R, Brughitta G, Lupattelli L. Does postcontrast MR enhancement in lumbar disc herniation have prognostic value. J Comput Assist Tomogr. 1995. 19:34–38.14. Komori H, Okawa A, Haro H, Muneta T, Yamamoto H, Shinomiya K. Contrast-enhanced magnetic resonance imaging in conservative management of lumbar disc herniations. Spine. 1998. 23:67–73.15. Buttermann GR. Lumbar disc herniation regression after successful epidural steroid injection. J Spinal Disord Tech. 2002. 15:469–476.16. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine. 1996. 21:225–229.17. Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the north american spine society, american society of spine radiology, and american society of neuroradiology. Spine. 2001. 26:E93–113.18. Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine. 1989. 14:431–437.19. Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar spinal disc herniations. Spine. 1990. 15:674–678.20. Haldeman S. North American Spine Society: failure of the pathology model to predict back pain. Spine. 1990. 15:718–724.21. Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. a prospective investigation. J Bone Joint Surg Am. 1990. 72:403–408.22. Rivest C, Katz N, Ferrante FM, Jamison RN. Effects of epidural steroid injection on pain due to lumbar spinal stenosis or herniated disks: a prospective study. Arthritis Care Res. 1998. 11:291–297.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report
- The Relationship between the Lower Lumbar Disc Herniation and the Morphology of the Iliolumbar Ligaments Using Magnetic Resonance Imaging
- Classification and Imaging Study of the Lumbar Disc Herniation
- Follow-up Magnetic Resonance Imaging Study of Patients with Herniated Lumbar Intervertebral Disc Who Were Treated Conservatively
- Ordinary Disc Herniation Changing into Posterior Epidural Migration of Lumbar Disc Fragments Confirmed by Magnetic Resonance Imaging: A Case Report of a Successful Endoscopic Treatment