Yonsei Med J.
2012 Mar;53(2):279-288. 10.3349/ymj.2012.53.2.279.
Electroanatomical Characteristics of Idiopathic Left Ventricular Tachycardia and Optimal Ablation Target during Sinus Rhythm: Significance of Preferential Conduction through Purkinje Fibers
- Affiliations
-
- 1Department of Cardiology, Yonsei University Health System, Seoul, Korea. hnpak@yuhs.ac
- 2Korea University Cardiovascular Center, Seoul, Korea.
- 3Utah Valley Regional Medical Center, Provo, UT and Krannert Heart Institute, Indiana University, Indianapolis, IN, USA.
- KMID: 1120193
- DOI: http://doi.org/10.3349/ymj.2012.53.2.279
Abstract
- PURPOSE
We hypothesized that Purkinje potential and their preferential conduction to the left ventricle (LV) posteroseptum during sinus rhythm (SR) are part of reentrant circuits of idiopathic left ventricular tachycardia (ILVT) and reentry anchors to papillary muscle.
MATERIALS AND METHODS
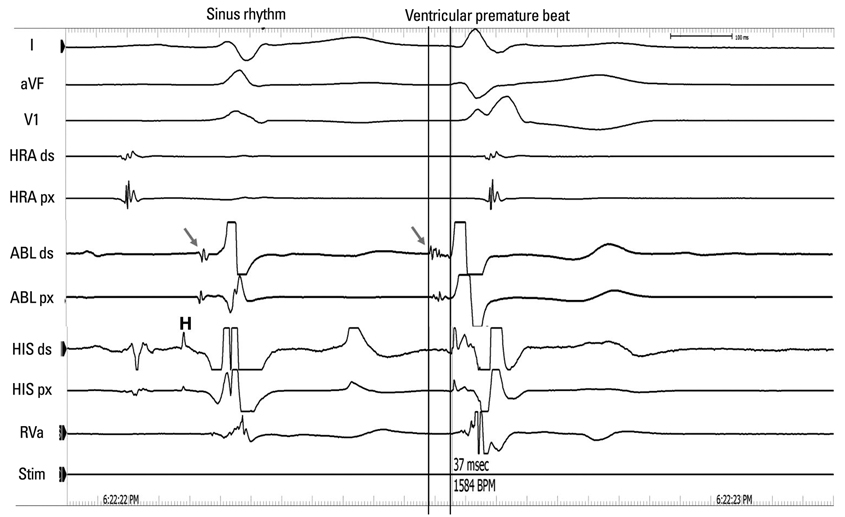
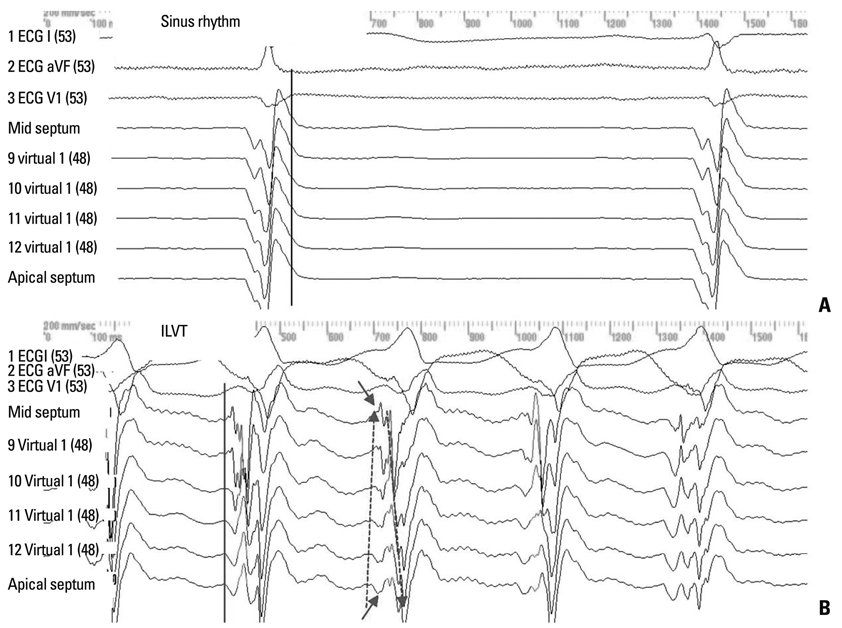
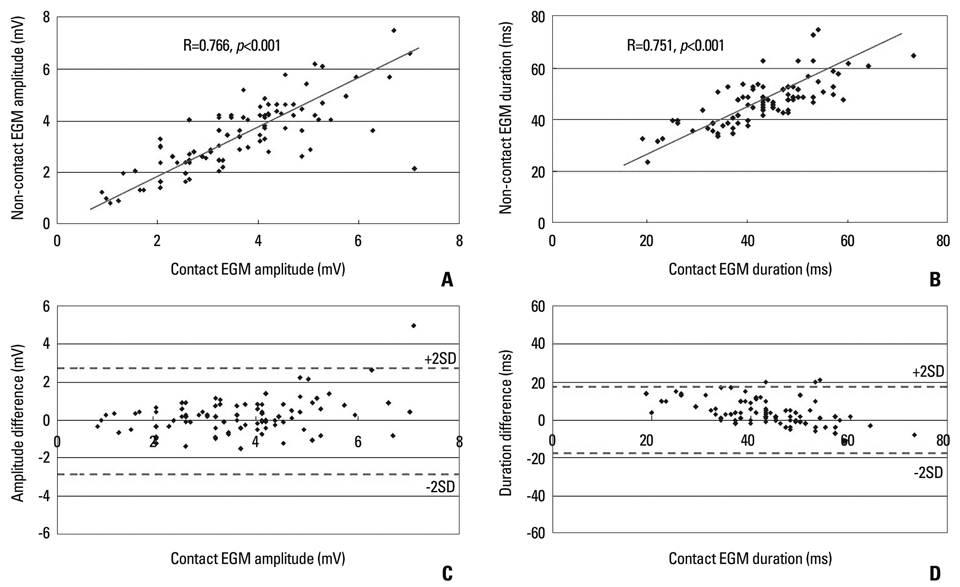
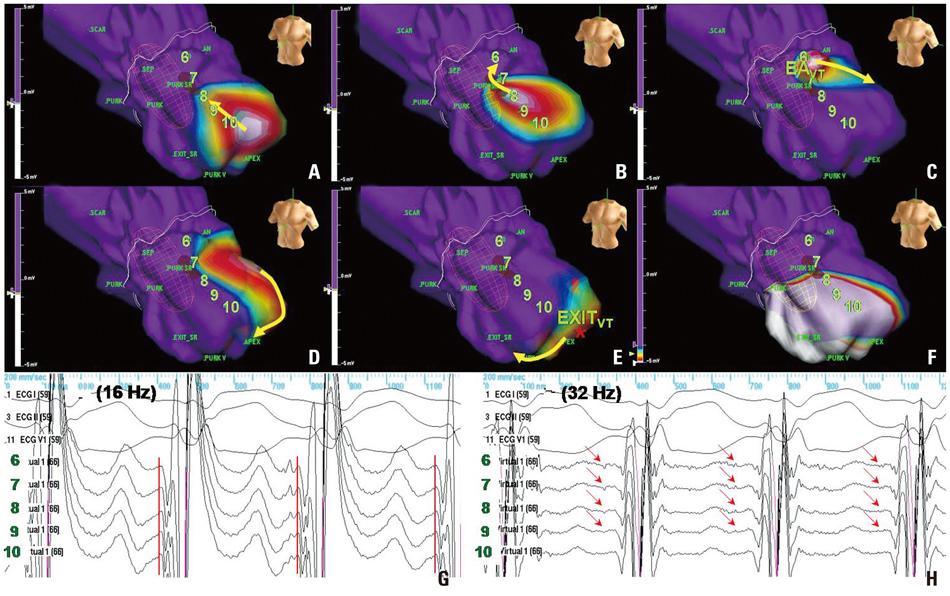
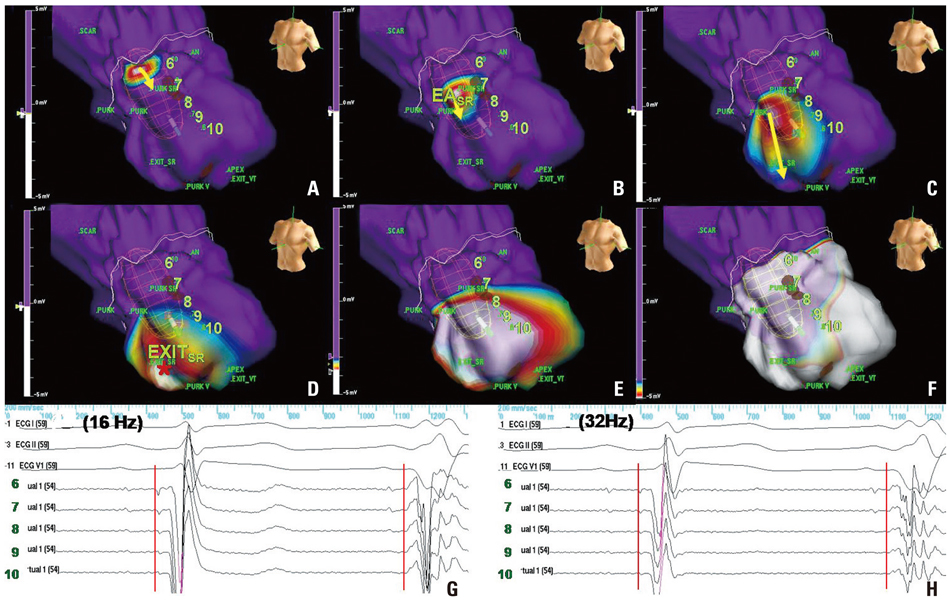
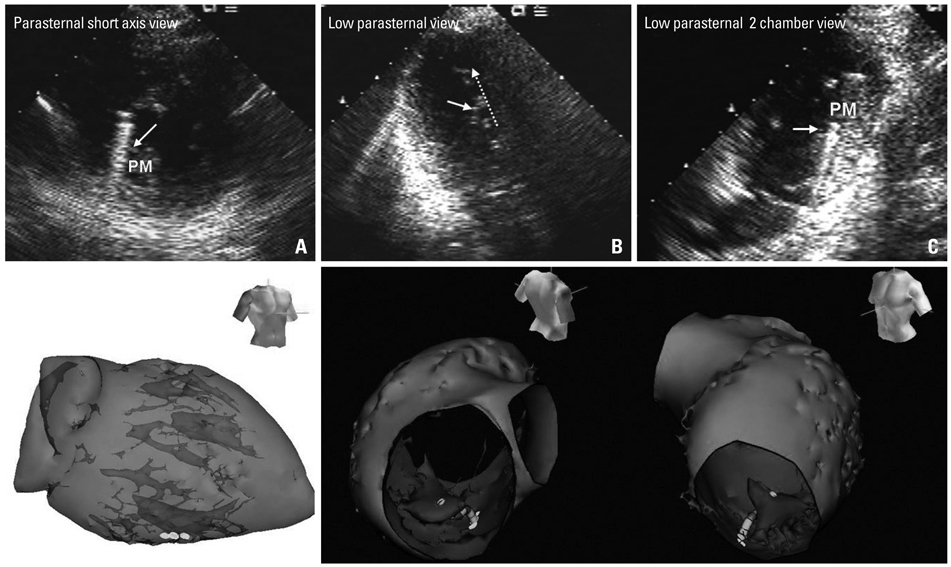
In 14 patients with ILVT (11 men, mean age 31.5+/-11.1 years), we compared Purkinje potential and preferential conduction during SR with VT by non-contact mapping (NCM). If clear Purkinje potential(SR) was observed in the LV posteroseptum and the earliest activation site (EA) of preferential conduction at SR (EASR) was well matched with that of VT (EAVT), EASR was targeted for radiofrequency catheter ablation (RFCA). Also, the anatomical locations of successful ablation sites were evaluated by echocardiography in five additional patients.
RESULTS
1) All induced VTs exhibited clear Purkinje potential(VT) and preferential conduction in the LV posteroseptum. The Purkinje potential(VT) and EAVT was within 5.8+/-8.2 mm of EASR. However, the breakout sites of VT were separated by 30.2+/-12.6 mm from EAVT to the apical side. 2) Purkinje potential(SR) demonstrated a reversed polarity to Purkinje potential(VT), and the interval of Purkinje potential(SR)-QRS was longer than the interval of Purkinje potential(VT)-QRS (p<0.02) 3) RFCA targeting EASR eliminated VT in all patients without recurrence within 23.3+/-7.5 months, and the successful ablation site was discovered at the base of papillary muscle in the five additional (100%) patients.
CONCLUSION
NCM-guided localization of EASR with Purkinje potential(SR) matches well with EAVT with Purkinje potential(VT) and provides an effective target for RFCA, potentially at the base of papillary muscle in patients with ILVT.
MeSH Terms
Figure
Reference
-
1. Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. 1981. 46:679–682.
Article2. Ouyang F, Cappato R, Ernst S, Goya M, Volkmer M, Hebe J, et al. Electroanatomic substrate of idiopathic left ventricular tachycardia: unidirectional block and macroreentry within the purkinje network. Circulation. 2002. 105:462–469.
Article3. Wen MS, Yeh SJ, Wang CC, Lin FC, Wu D. Successful radiofrequency ablation of idiopathic left ventricular tachycardia at a site away from the tachycardia exit. J Am Coll Cardiol. 1997. 30:1024–1031.
Article4. Nakagawa H, Beckman KJ, McClelland JH, Wang X, Arruda M, Santoro I, et al. Radiofrequency catheter ablation of idiopathic left ventricular tachycardia guided by a Purkinje potential. Circulation. 1993. 88:2607–2617.
Article5. Nogami A, Naito S, Tada H, Taniguchi K, Okamoto Y, Nishimura S, et al. Demonstration of diastolic and presystolic Purkinje potentials as critical potentials in a macroreentry circuit of verapamil-sensitive idiopathic left ventricular tachycardia. J Am Coll Cardiol. 2000. 36:811–823.
Article6. Doppalapudi H, Yamada T, McElderry HT, Plumb VJ, Epstein AE, Kay GN. Ventricular tachycardia originating from the posterior papillary muscle in the left ventricle: a distinct clinical syndrome. Circ Arrhythm Electrophysiol. 2008. 1:23–29.
Article7. Blanchard SM, Damiano RJ Jr, Smith WM, Ideker RE, Lowe JE. Interpolating unipolar epicardial potentials from electrodes separated by increasing distances. Pacing Clin Electrophysiol. 1989. 12:1938–1955.
Article8. Swartz JF, Tracy CM, Fletcher RD. Radiofrequency endocardial catheter ablation of accessory atrioventricular pathway atrial insertion sites. Circulation. 1993. 87:487–499.
Article9. Friedman PA, Asirvatham SJ, Grice S, Glikson M, Munger TM, Rea RF, et al. Noncontact mapping to guide ablation of right ventricular outflow tract tachycardia. J Am Coll Cardiol. 2002. 39:1808–1812.
Article10. Sra J, Bhatia A, Krum D, Akhtar M. Endocardial noncontact activation mapping of idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol. 2000. 11:1409–1412.
Article11. Betts TR, Roberts PR, Allen SA, Morgan JM. Radiofrequency ablation of idiopathic left ventricular tachycardia at the site of earliest activation as determined by noncontact mapping. J Cardiovasc Electrophysiol. 2000. 11:1094–1101.
Article12. Schilling RJ, Peters NS, Davies DW. Simultaneous endocardial mapping in the human left ventricle using a noncontact catheter: comparison of contact and reconstructed electrograms during sinus rhythm. Circulation. 1998. 98:887–898.
Article13. Higa S, Tai CT, Lin YJ, Liu TY, Lee PC, Huang JL, et al. Focal atrial tachycardia: new insight from noncontact mapping and catheter ablation. Circulation. 2004. 109:84–91.
Article14. Maruyama M, Tadera T, Miyamoto S, Ino T. Demonstration of the reentrant circuit of verapamil-sensitive idiopathic left ventricular tachycardia: direct evidence for macroreentry as the underlying mechanism. J Cardiovasc Electrophysiol. 2001. 12:968–972.
Article15. Okumura K, Matsuyama K, Miyagi H, Tsuchiya T, Yasue H. Entrainment of idiopathic ventricular tachycardia of left ventricular origin with evidence for reentry with an area of slow conduction and effect of verapamil. Am J Cardiol. 1988. 62:727–732.
Article16. Tsuchiya T, Okumura K, Honda T, Honda T, Iwasa A, Yasue H, et al. Significance of late diastolic potential preceding Purkinje potential in verapamil-sensitive idiopathic left ventricular tachycardia. Circulation. 1999. 99:2408–2413.
Article17. Massing GK, James TN. Anatomical configuration of the His bundle and bundle branches in the human heart. Circulation. 1976. 53:609–621.
Article18. Tsuchiya T, Okumura K, Honda T, Iwasa A, Ashikaga K. Effects of verapamil and lidocaine on two components of the re-entry circuit of verapamil-senstitive idiopathic left ventricular tachycardia. J Am Coll Cardiol. 2001. 37:1415–1421.
Article19. Ma FS, Ma J, Tang K, Han H, Jia YH, Fang PH, et al. Left posterior fascicular block: a new endpoint of ablation for verapamil-sensitive idiopathic ventricular tachycardia. Chin Med J (Engl). 2006. 119:367–372.20. Lee KT, Chu CS, Dai ZK, Wu JR, Sheu SH, Lai WT. Successful catheter ablation of idiopathic left ventricular tachycardia during sinus rhythm. Int J Cardiol. 2007. 115:e74–e77.
Article21. Chen M, Yang B, Zou J, Shan Q, Chen C, Xu D, et al. Non-contact mapping and linear ablation of the left posterior fascicle during sinus rhythm in the treatment of idiopathic left ventricular tachycardia. Europace. 2005. 7:138–144.
Article22. Chen PS, Karagueuzian HS, Kim YH. Papillary muscle hypothesis of idiopathic left ventricular tachycardia. J Am Coll Cardiol. 2001. 37:1475–1476.
Article23. Joyner RW, Ramza BM, Tan RC. Effects of stimulation frequency on Purkinje-ventricular conduction. Ann N Y Acad Sci. 1990. 591:38–50.
Article24. Kim YH, Xie F, Yashima M, Wu TJ, Valderrábano M, Lee MH, et al. Role of papillary muscle in the generation and maintenance of reentry during ventricular tachycardia and fibrillation in isolated swine right ventricle. Circulation. 1999. 100:1450–1459.
Article25. Myerburg RJ, Nilsson K, Gelband H. Physiology of canine intraventricular conduction and endocardial excitation. Circ Res. 1972. 30:217–243.
Article26. Veenstra RD, Joyner RW, Rawling DA. Purkinje and ventricular activation sequences of canine papillary muscle. Effects of quinidine and calcium on the Purkinje-ventricular conduction delay. Circ Res. 1984. 54:500–515.
Article27. Haïssaguerre M, Shoda M, Jaïs P, Nogami A, Shah DC, Kautzner J, et al. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002. 106:962–967.
Article28. Pak HN, Oh YS, Liu YB, Wu TJ, Karagueuzian HS, Lin SF, et al. Catheter ablation of ventricular fibrillation in rabbit ventricles treated with beta-blockers. Circulation. 2003. 108:3149–3156.
Article29. Pak HN, Kim YH, Lim HE, Chou CC, Miyauchi Y, Fang YH, et al. Role of the posterior papillary muscle and purkinje potentials in the mechanism of ventricular fibrillation in open chest dogs and Swine: effects of catheter ablation. J Cardiovasc Electrophysiol. 2006. 17:777–783.
Article30. Good E, Desjardins B, Jongnarangsin K, Oral H, Chugh A, Ebinger M, et al. Ventricular arrhythmias originating from a papillary muscle in patients without prior infarction: a comparison with fascicular arrhythmias. Heart Rhythm. 2008. 5:1530–1537.
Article31. Yamada T, Doppalapudi H, McElderry HT, Okada T, Murakami Y, Inden Y, et al. Electrocardiographic and electrophysiological characteristics in idiopathic ventricular arrhythmias originating from the papillary muscles in the left ventricle: relevance for catheter ablation. Circ Arrhythm Electrophysiol. 2010. 3:324–331.
Article32. Song PS, Kim JS, Shin DH, Park JW, Bae KI, Lee CH, et al. Electrical storms in patients with an implantable cardioverter defibrillator. Yonsei Med J. 2011. 52:26–32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Supraventricular Tachycardia and Sinus Rhythm with Contralateral Bundle Branch Block Patterns
- The Significance of Repetitive Ventricular Responses Induced by Radiofrequency Energy Application for Idiopathic Left Ventricular Tachycardia
- Beta Blocker Sensitive Idiopathic Ventricular Tachycardia
- Unsolved Questions on the Anatomy of the Ventricular Conduction System
- Successful Catheter Ablation of Focal Automatic Left Ventricular Tachycardia Presented with Tachycardia-Mediated Cardiomyopathy