J Korean Acad Nurs.
2011 Dec;41(6):788-794. 10.4040/jkan.2011.41.6.788.
Heart Rate Variability and Metabolic Syndrome in Hospitalized Patients with Schizophrenia
- Affiliations
-
- 1College of Nursing, Keimyung University, Daegu, Korea. khl645@kmu.ac.kr
- 2Department of Nursing, Gyeongsan University College, Gyeongsan, Korea.
- 3Keimyung University Dongsan Medical Center, Daegu, Korea.
- 4College of Nursing, University of Illinois at Chicago, USA.
- KMID: 1120111
- DOI: http://doi.org/10.4040/jkan.2011.41.6.788
Abstract
- PURPOSE
Reduced heart rate variability significantly increases cardiovascular mortality. Metabolic syndrome increases the cardiac autonomic dysfunction. Recently, increasing cardiovascular mortality has been reported in patients with schizophrenia. This study was done to compare heart rate variability between adults with and without schizophrenia and to compare the relationship of heart rate variability to metabolic syndrome in hospitalized patients with schizophrenia.
METHODS
This was a descriptive and correlational study in which 719 adults without schizophrenia and 308 adults with schizophrenia took part between May and June 2008. We measured the following: five-minute heart rate variability; high-frequency, low-frequency, the ratio of low-frequency to high-frequency, and the Standard Deviation of all the normal RR intervals. Data was also collected on metabolic syndrome, abdominal obesity, triglycerides, HDL cholesterol, blood pressure and fasting glucose.
RESULTS
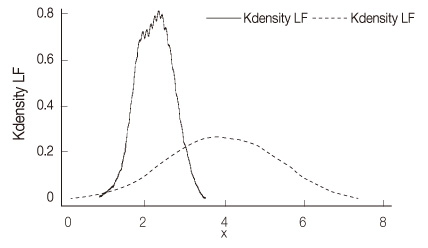
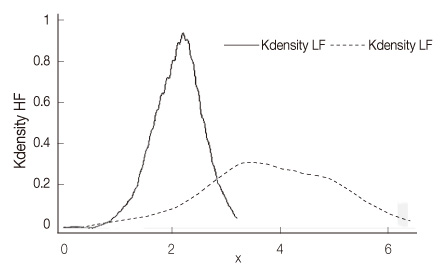
The Standard Deviation of all the normal RR intervals values of heart rate variability indices were 1.53+/-0.18. The low-frequency and high-frequency values of heart rate variability indices were significantly higher in hospitalized patients with schizophrenia (3.89+/-1.36; 3.80+/-1.20) than those in the healthy participants (2.20+/-0.46; 2.10+/-0.46). There were no significant differences between the schizophrenic patients with and without metabolic syndrome.
CONCLUSION
The results of this study indicate that schizophrenia patients have significantly lower cardiac autonomic control, but they have significantly higher low-frequency and high-frequency values than those of healthy adults. Use of antipsychotic drug may affect the autonomic nervous system in schizophrenic patients. Metabolic syndrome was not associated with cardiac autonomic control in schizophrenia patients.
Keyword
MeSH Terms
-
Adult
Autonomic Nervous System/physiopathology
Blood Glucose/analysis
Blood Pressure
Cardiovascular Diseases/complications/diagnosis/mortality
Cholesterol, HDL/blood
Female
*Heart Rate
Hospitalization
Humans
Male
Metabolic Syndrome X/*complications/*physiopathology
Middle Aged
Obesity/etiology
Schizophrenia/*complications/mortality/*physiopathology
Triglycerides/blood
Figure
Cited by 2 articles
-
Factors Influencing Metabolic Syndrome among Mental Health Facility Patients with Schizophrenia
Sun-Hye Lee, Sunhee Cho
J Korean Acad Psychiatr Ment Health Nurs. 2016;25(1):1-10. doi: 10.12934/jkpmhn.2016.25.1.1.Factors Influencing Metabolic Syndrome among Mental Health Facility Patients with Schizophrenia
Sun-Hye Lee, Sunhee Cho
J Korean Acad Psychiatr Ment Health Nurs. 2016;25(1):1-10. doi: 10.12934/jkpmhn.2016.25.1.1.
Reference
-
1. Agelink MW, Majewski T, Wurthmann C, Lukas K, Ullrich H, Linka T, et al. Effects of newer atypical antipsychotics on autonomic neurocardiac function: A comparison between amisulpride, olanzapine, sertindole, and clozapine. Journal of Clinical Psychopharmacology. 2001. 21:8–13.2. Astrup AS, Tarnow L, Rossing P, Hansen BV, Hilsted J, Parving HH. Cardiac autonomic neuropathy predicts cardiovascular morbidity and mortality in type 1 diabetic patients with diabetic nephropathy. Diabetes Care. 2006. 29:334–339. doi: 10.2337/diacare.29.02.06.dc05-1242.3. Bar KJ, Letzsch A, Jochum T, Wagner G, Greiner W, Sauer H. Loss of efferent vagal activity in acute schizophrenia. Journal of Psychiatric Research. 2005. 39:519–527.4. Birkhofer A, Alger P, Schmid G, Forstl H. The cardiovascular risk of schizophrenic patients. Neuropsychiatr. 2007. 21:261–266.5. Boettger S, Hoyer D, Falkenhahn K, Kaatz M, Yeragani VK, Bar KJ. Altered diurnal autonomic variation and reduced vagal information flow in acute schizophrenia. Clinical Neurophysiology. 2006. 117:2715–2722. doi: 10.1016/j.clinph.2006.08.009.6. Cohen H, Loewenthal U, Matar M, Kotler M. Association of autonomic dysfunction and clozapine. Heart rate variability and risk for sudden death in patients with schizophrenia on long-term psychotropic medication. The British Journal of Psychiatry. 2001. 179:167–171.7. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004. 110:227–239.8. Henry BL, Minassian A, Paulus MP, Geyer MA, Perry W. Heart rate variability in bipolar mania and schizophrenia. Journal of Psychiatric Research. 2010. 44:168–176. doi: 10.1016/j.jpsychires.2009.07.011.9. Ikawa M, Tabuse H, Ueno S, Urano T, Sekiya M, Murakami T. Effects of combination psychotropic drug treatment on heart rate variability in psychiatric patients. Psychiatry and Clinical Neurosciences. 2001. 55:341–345. doi: 10.1046/j.1440-1819.2001.00873.x.10. Karason K, Molgaard H, Wikstrand J, Sjostrom L. Heart rate variability in obesity and the effect of weight loss. American Journal of Cardiology. 1999. 83:1242–1247. doi: 10.1016/S0002-9149(99)00066-1.11. Kelly DL, McMahon RP, Liu F, Love RC, Wehring HJ, Shim JC, et al. Cardiovascular disease mortality in patients with chronic schizophrenia treated with clozapine: A retrospective cohort study. Journal of Clinical Psychiatry. 2010. 71:304–311. doi: 10.4088/JCP.08m04718yel.12. Kim JA, Park YG, Cho KH, Hong MH, Han HC, Choi YS, et al. Heart rate variability and obesity indices: Emphasis on the response to noise and standing. Journal of the American Board of Family Practice. 2005. 18:97–103. doi: 10.1152/japplphysiol.01275.2005.13. Kuch B, Hense HW, Sinnreich R, Kark JD, von Eckardstein A, Sapoznikov D, et al. Determinants of short-period heart rate variability in the general population. Cardiology. 2001. 95:131–138.14. Kudat H, Akkaya V, Sozen AB, Salman S, Demirel S, Ozcan M, et al. Heart rate variability in diabetes patients. Journal of International Medical Research. 2006. 34:291–296.15. La Rovere MT, Bigger JT Jr, Marcus FI, Mortara A, Schwartz PJ. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet. 1998. 351:478–484. doi: 10.1016/S0140-6736(97)11144-8.16. La Rovere MT, Pinna GD, Hohnloser SH, Marcus FI, Mortara A, Nohara R, et al. Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: Implications for clinical trials. Circulation. 2001. 103:2072–2077.17. Lee WY, Park JS, Noh SY, Rhee EJ, Kim SW, Zimmet PZ. Prevalence of the metabolic syndrome among 40,698 Korean metropolitan subjects. Diabetes Research and Clinical Practice. 2004. 65:143–149.18. Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G. Lower heart rate variability is associated with the development of coronary heart disease in individuals with diabetes: The atherosclerosis risk in communities (ARIC) study. Diabetes. 2002. 51:3524–3531.19. Mann K, Rossbach W, Muller MJ, Muller-Siecheneder F, Ru H, Dittmann RW. Heart rate variability during sleep in patients with schizophrenia treated with olanzapine. International Clinical Psychopharmacology. 2004. 19:325–330.20. McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, Sullivan L, et al. Prevalence of the metabolic syndrome in patients with schizophrenia: Baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schizophrenia Research. 2005. 80:19–32. doi: 10.1016/j.schres.2005.07.014.21. Meyer JM. Effects of atypical antipsychotics on weight and serum lipid levels. Journal of Clinical Psychiatry. 2001. 62:27–34.22. Meyer JM, Nasrallah HA, McEvoy JP, Goff DC, Davis SM, Chakos M, et al. The Clinical Antipsychotic trials Of Intervention Effectiveness (CATIE) Schizophrenia trial: Clinical comparison of subgroups with and without the metabolic syndrome. Schizophrenia Research. 2005. 80:9–18. doi: 10.1016/j.schres.2005.07.015.23. Montano N, Gneddhi RT, Porta A, Lombardi F, Pagani M, Malliani A. Power spectrum analysis of heart rate variability to assess the changes in sympathovagal balance during graded orthostatic tilt. Circulation. 1994. 90:1826–1831.24. Oh JY, Hong YS, Sung YA, Barrett-Connor E. Prevalence and factor analysis of metabolic syndrome in an urban Korean population. Diabetes Care. 2004. 27:2027–2032. doi: 10.2337/diacare.27.8.2027.25. Sugawara N, Yasui-Furukori N, Sato Y, Kishida I, Yamashita H, Saito M, et al. Comparison of prevalence of metabolic syndrome in hospital and community-based Japanese patients with schizophrenia. Annals of General Psychiatry. 2011. 10:21. doi: 10.1186/1744-859X-10-21.26. Suvisaari JM, Saarni SI, Perala J, Suvisaari JV, Harkanen T, Lonnqvist J, et al. Metabolic syndrome among persons with schizophrenia and other psychotic disorders in a general population survey. Journal of Clinical Psychiatry. 2007. 68:1045–1055.27. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation. 1996. 93:1043–1065.28. Van Ravenswaaij-Arts CM, Kollee LA, Hopman JC, Stoelinga GB, van Geijn HP. Heart rate variability. Annals of Internal Medicine. 1993. 118:436–447.29. WHO, IASO, & IOTF. The Asia-Pacific perspective: Redefining obesity and its treatment. 2000. Australia: Health Communications;1–56.30. Wang YC, Yang CC, Bai YM, Kuo TB. Heart rate variability in schizophrenic patients switched from typical antipsychotic agents to amisulpride and olanzapine: 3-month follow-up. Neuropsychobiology. 2008. 57:200–205. doi: 10.1159/000149818.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Heart Rate Variability and Metabolic Syndrome at a Rural Area
- Effect of Yoga on Heart Rate Variability in Women with Metabolic Syndrome
- Association between Heart Rate Variability and Metabolic Syndrome
- Prevalence of the Metabolic Syndrome among Outpatients with Schizophrenia or Schizoaffective Disorder
- Heart Rate Variability in Psychiatry