Korean J Radiol.
2008 Jul;9(Suppl):S1-S6. 10.3348/kjr.2008.9.s.s1.
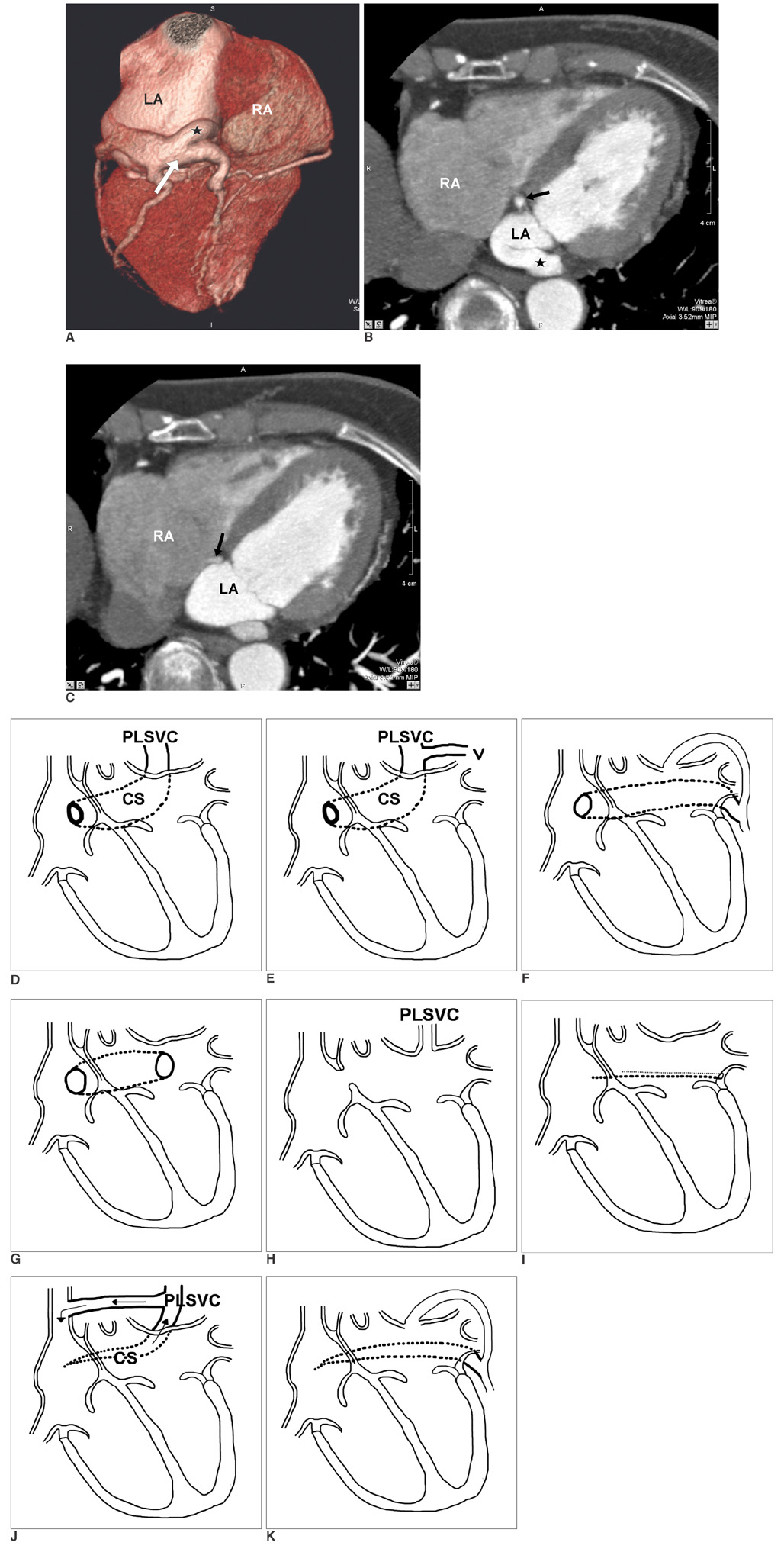
Multidetector CT Findings of a Congenital Coronary Sinus Anomaly: a Report of Two Cases
- Affiliations
-
- 1Department of Radiology, Yong-Kang Campus, Chi-Mei Medical Center, Taiwan, R.O.C. meichuntw@yahoo.com
- 2Section of Thoracic and Circulation Imaging, Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, R.O.C.
- 3Faculty of medicine, School of medicine, National Yang Ming University, Taipei, Taiwan, R.O.C.
- 4Department of Radiology, National Defense Medical Center, Taiwan, R.O.C.
- 5Department of Radiological Technology, Central Taiwan University of Science and Technology, Taichung, Taiwan, R.O.C.
- KMID: 1100093
- DOI: http://doi.org/10.3348/kjr.2008.9.s.s1
Abstract
- Congenital coronary sinus anomalies are extremely rare, and they have received relatively little attention. This is probably due to the lack of both clinical symptoms and significant cardiac functional disturbance. We present two cases of a coronary sinus anomaly and briefly review the literature. Recognizing and being familiar with the variations of a congenital coronary sinus anomaly in congenital heart disease may avoid a misinterpretation of cardiac catheterization findings and the troublesome disruption of coronary sinus blood return during the surgical management of cardiac lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Mantini E, Grondin CM, Lillehei CW, Edwards JE. Congenital anomalies involving the coronary sinus. Circulation. 1966. 33:317–327.2. Ruengsakulrach P, Buxton BF. Anatomic and hemodynamic considerations influencing the efficiency of retrograde cardioplegia. Ann Thorac Surg. 2001. 71:1389–1395.3. Jha NK, Gogna A, Tan TH, Wong KY, Shankar S. Atresia of coronary sinus ostium with retrograde drainage via persistent left superior vena cava. Ann Thorac Surg. 2003. 76:2091–2092.4. Rose AG, Beckman CB, Edwards JE. Communication between coronary sinus and left atrium. Br Heart J. 1974. 36:182–185.5. Miraldi F, di Gioia CR, Proietti P, De Santis M, d'Amati G, Gallo P. Cardinal vein isomerism: an embryological hypothesis to explain a persistent left superior vena cava draining into the roof of the left atrium in the absence of coronary sinus and atrial septal defect. Cardiovasc Pathol. 2002. 11:149–152.6. Neuser H, Kerber S, Schumacher B. Images in cardiovascular medicine. Fistulous communication between coronary sinus and left atrium. Circulation. 2002. 106:E137–E138.7. Edwards JE, DuShane JW. Thoracic venous anomalies. Arch Pathol. 1950. 49:517–537.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum
- A Single Coronary Artery with the Right Coronary Artery Originating from the Left Anterior Descending Artery Detected by Cardiac CT: A Case Report
- Acute Myocardial Infarction in Patients With Single Coronary Artery: A Case Report
- Anomalous Origin of the Left Circumflex Coronary Artery from the Right Sinus of Valsalva Identified by Imaging with Multidetector Computed Tomography
- Congenital Anomalies of the Coronary Sinus: A Pictorial Essay