Korean J Lab Med.
2011 Jan;31(1):18-21. 10.3343/kjlm.2011.31.1.18.
A Case of Monoclonal Gammopathy in Extranodal Marginal Zone B-cell Lymphoma of the Small Intestine
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 2Department of Laboratory Medicine, College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea. rocky@dumc.or.kr
- 3Department of Pathology, College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 4Department of Nuclear Medicine, College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- 5Department of Surgery, College of Medicine, Dongguk University Ilsan Hospital, Goyang, Korea.
- KMID: 1096655
- DOI: http://doi.org/10.3343/kjlm.2011.31.1.18
Abstract
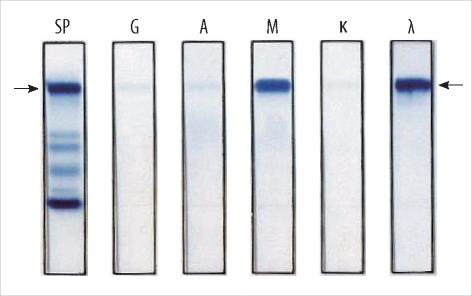
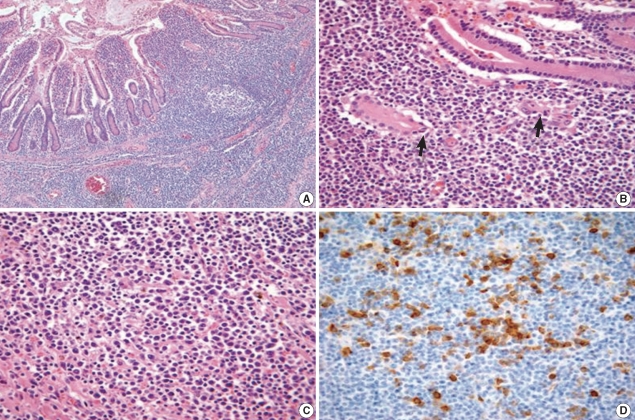
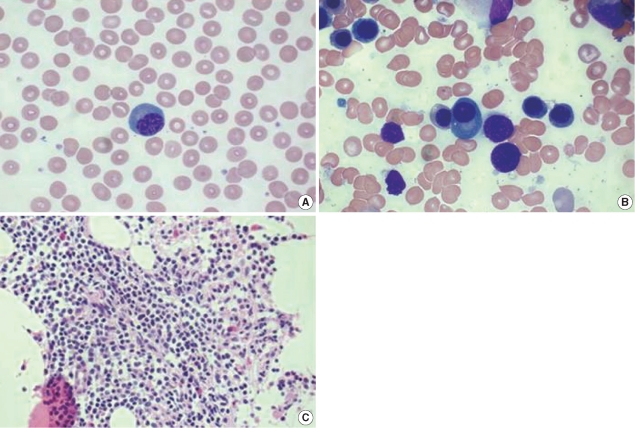
- Monoclonal gammopathy occurs in one-third of the patients with mucosa-associated lymphoid tissue lymphoma (MALT lymphoma). However, monoclonal gammopathy has been rarely reported in Korea. Paraprotenemia accompanying MALT lymphoma is strongly correlated with involvement of the bone marrow, and this involvement leads to the progression of the disease. Here, we present a case of a 66-yr-old man diagnosed with IgM monoclonal gammopathy and stage IV extranodal marginal zone lymphoma of the small intestine, with the involvement of the bone marrow.
MeSH Terms
-
Aged
Antineoplastic Agents/therapeutic use
Bone Marrow/pathology
Drug Therapy, Combination
Electrophoresis, Polyacrylamide Gel
Humans
Immunoglobulin M/analysis
Intestinal Neoplasms/complications/drug therapy/*pathology
Lymphatic Metastasis
Lymphoma, B-Cell, Marginal Zone/complications/drug therapy/*pathology
Male
Neoplasm Staging
Paraproteinemias/blood/complications/*pathology
Positron-Emission Tomography
Tomography, X-Ray Computed
Figure
Reference
-
1. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood. 1997; 89:3909–3918. PMID: 9166827.2. Raderer M, Streubel B, Woehrer S, Puespoek A, Jaeger U, Formanek M, et al. High relapse rate in patients with MALT lymphoma warrants lifelong follow-up. Clin Cancer Res. 2005; 11:3349–3352. PMID: 15867234.3. Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000; 95:802–806. PMID: 10648389.
Article4. Tirelli A, Guastafierro S, Cava B, Lucivero G. Triclonal gammopathy in an extranodal non-Hodgkin lymphoma patient. Am J Hematol. 2003; 73:273–275. PMID: 12879432.
Article5. Tursi A, Modeo ME. Monoclonal gammopathy of undetermined significance predisposing to Helicobacter pylori-related gastric mucosa-associated lymphoid tissue lymphoma. J Clin Gastroenterol. 2002; 34:147–149. PMID: 11782609.6. Yamasaki S, Matsushita H, Tanimura S, Nakatani T, Hara S, Endo Y, et al. B-cell lymphoma of mucosa-associated lymphoid tissue of the thymus: a report of two cases with a background of Sjögren's syndrome and monoclonal gammopathy. Hum Pathol. 1998; 29:1021–1024. PMID: 9744322.7. Wöhrer S, Streubel B, Bartsch R, Chott A, Raderer M. Monoclonal immunoglobulin production is a frequent event in patients with mucosa-associated lymphoid tissue lymphoma. Clin Cancer Res. 2004; 10:7179–7181. PMID: 15534090.
Article8. Asatiani E, Cohen P, Ozdemirli M, Kessler CM, Mavromatis B, Cheson BD. Monoclonal gammopathy in extranodal marginal zone lymphoma (ENMZL) correlates with advanced disease and bone marrow involvement. Am J Hematol. 2004; 77:144–146. PMID: 15389912.
Article9. Hwang EK, Jang EJ, Kim SM, Jeong SH, Lee HW, Kang SY, et al. A case report of Helicobacter pylori negative gastric MALT lymphoma with monoclonal gammopathy. Korean J Hematol. 2009; 44:261–267.10. Ott MM, Rosenwald A, Katzenberger T, Dreyling M, Krumdiek AK, Kalla J, et al. Marginal zone B-cell lymphomas (MZBL) arising at different sites represent different biological entities. Genes Chromosomes Cancer. 2000; 28:380–386. PMID: 10862046.
Article11. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. 2008. 4th ed. Lyon: International Agency for Research on Cancer;p. 214–216.12. Deegan MJ, Abraham JP, Sawdyk M, Van Slyck EJ. High incidence of monoclonal proteins in the serum and urine of chronic lymphocytic leukemia patients. Blood. 1984; 64:1207–1211. PMID: 6437461.
Article13. Catovsky D, Matutes E. Splenic lymphoma with circulating villous lymphocytes/splenic marginal-zone lymphoma. Semin Hematol. 1999; 36:148–154. PMID: 10319383.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Marginal Zone B-cell Lymphoma of MALT in Small Intestine Associated with Amyloidosis: A Rare Association
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- Clinical Study of Ocular Adnexal Extranodal Marginal Zone B-cell Lymphoma: From the Perspective of Dermatology
- A case of nodal marginal zone B-cell lymphoma of the lower eyelid
- A Case of Primary Cutaneous Marginal Zone B-cell Lymphoma