Yonsei Med J.
2010 Sep;51(5):717-721. 10.3349/ymj.2010.51.5.717.
Infantile Vulvar Abscess with a Normal Anus: A Suspicious Sign of Rectovestibular Fistula
- Affiliations
-
- 1Department of Surgery, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea.
- 2Department of Pediatric Surgery, Dankook University Medical College, Cheonan, Korea.
- 3Department of Pediatric Surgery, Hallym University Sacred Medical Center, Hallym University College of Medicine, Anyang, Korea.
- 4Department of Pediatric Surgery, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. sjhan@yuhs.ac
- KMID: 1071423
- DOI: http://doi.org/10.3349/ymj.2010.51.5.717
Abstract
- PURPOSE
We investigated whether infantile vulvar abscesses are predictable features of rectovestibular fistula with a normal anus.
MATERIALS AND METHODS
A retrospective analysis of five infants with vulvar abscesses and rectovestibular fistulae with normal anuses was performed.
RESULTS
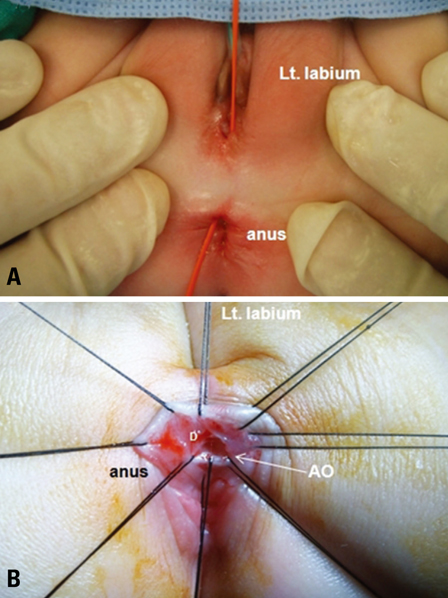
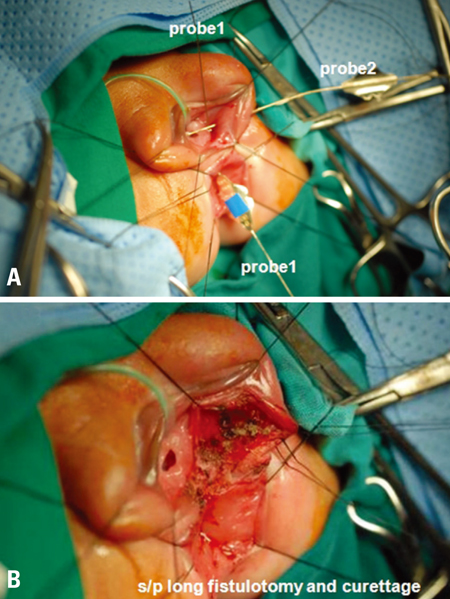
Four cases had a left vulvar abscess, and in one case the vulvar abscess was on the right side. All caregivers reported passage of stool from the vagina. The fistulae were almost uniformly located from the vestibule to the rectum above the anal dentate line, observable by visual inspection and probing under anesthesia. The first two cases were treated with division and closure of the fistulae after a diverting loop colostomy, and the remaining three cases with fistulotomy and curettage. There was no recurrence during the median follow-up period of 38 months.
CONCLUSION
This unique rectovestibular fistula should be suspected in female infants with vulvar abscesses, especially when parents report passage of stool from the vagina. Fistulotomy and curettage may be an initial treatment and effective as a temporary diverting colostomy and delayed repair of the fistula.
MeSH Terms
Figure
Reference
-
1. Bryndorf J, Madsen CM. Ectopic anus in the female. Acta Chir Scand. 1960. 118:466–478.2. Petit T, Fouques Y, Viatounou S, Mesnil JL, Ravasse P. [Congenital rectovestibular fistula. An unusual diagnosis that should not be ignored]. Arch Pediatr. 2002. 9:595–597.3. Mirza I, Zia-ul-Miraj M. Management of perineal canal anomaly. Pediatr Surg Int. 1997. 12:611–612.
Article4. Meyer T, Höcht B. [Congenital H-type anorectal fistula: two case reports]. Klin Padiatr. 2009. 221:38–40.5. Tsuchida Y, Saito S, Honna T, Makino S, Kaneko M, Hazama H. Double termination of the alimentary tract in females: a report of 12 cases and a literature review. J Pediatr Surg. 1984. 19:292–296.
Article6. Akhparov NN, Aipov RR, Ormantayev KS. The surgical treatment of H-fistula with normal anus in girls. Pediatr Surg Int. 2008. 24:1207–1210.
Article7. Rintala RJ, Mildh L, Lindahl H. H-type anorectal malformations: incidence and clinical characteristics. J Pediatr Surg. 1996. 31:559–562.
Article8. Wakhlu A, Pandey A, Prasad A, Kureel SN, Tandon RK, Wakhlu AK. Perineal canal. Pediatr Surg Int. 1997. 12:283–285.
Article9. White JJ, Haller JA Jr, Scott JR, Dorst JP, Kramer SS. N-type anorectal malformations. J Pediatr Surg. 1978. 13:631–637.
Article10. Holschneider A, Hutson J, Peña A, Beket E, Chatterjee S, Coran A, et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J Pediatr Surg. 2005. 40:1521–1526.
Article11. Yazlcl M, Etensel B, Gürsoy H, Ozklsaclk S. Congenital H-type anovestibuler fistula. World J Gastroenterol. 2003. 9:881–882.
Article12. Banu T, Hannan MJ, Hoque M, Aziz MA, Lakhoo K. Anovestibular fistula with normal anus. J Pediatr Surg. 2008. 43:526–529.
Article13. Chatterjee SK. Double termination of the alimentary tract--a second look. J Pediatr Surg. 1980. 15:623–627.
Article14. Chen YJ, Zhang TC, Zhang JZ. Transanal approach in repairing acquired rectovestibular fistula in females. World J Gastroenterol. 2004. 10:2299–2300.
Article15. Borgstein ES, Broadhead RL. Acquired rectovaginal fistula. Arch Dis Child. 1994. 71:165–166.
Article16. Wiersma R. HIV-positive African children with rectal fistulae. J Pediatr Surg. 2003. 38:62–64.
Article17. Hyde GA Jr, Sarbah S. Acquired rectovaginal fistula in human immunodeficiency virus-positive children. Pediatrics. 1994. 94:940–941.
Article18. Li L, Zhang TC, Zhou CB, Pang WB, Chen YJ, Zhang JZ. Rectovestibular fistula with normal anus: a simple resection or an extensive perineal dissection? J Pediatr Surg. 2010. 45:519–524.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and Treatment of Congenital H-type Rectovestibular Fistula
- Tubular Colonic Duplication Presenting as Rectovestibular Fistula
- A Case of Perineal Hemangioma, External Genitalia Malformations, Lipomyelomeningocele, Vesicorenal Abnormalities, Imperforate Anus, and Skin Tag (PELVIS) Syndrome with Extensive Perineal Infantile Hemangioma
- Two Experiences of Operation about Urogenital Anomalies Associated with Congenital Imperforate Anus
- A Clinical Study of Fistula-in-Ano and Perianal Abscess in Childhood