J Korean Soc Spine Surg.
2010 Dec;17(4):184-190. 10.4184/jkss.2010.17.4.184.
Management of Deep Wound Infection After Posterior Lumbar Interbody Fusion With Cages
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Bucheon Hospital, Korea. eungha@unitel.co.kr
- KMID: 2209581
- DOI: http://doi.org/10.4184/jkss.2010.17.4.184
Abstract
- STUDY DESIGN: Retrospective study
OBJECTIVES
The purpose of this study was to analyze patients who developed deep wound infections after receiving PLIF for degenerative lumbar disease, and report the treatment outcomes. SUMMARY OF LITERATURE REVIEW: Few studies have examined deep wound infections after PLIF, and there is some controversy regarding whether screws or cages need to be removed to treat infections.
MATERIALS AND METHODS
Nine cases(spinal stenosis 6, spondylolisthesis 3) developed a deep wound infection after PLIF from 2001 to 2007. The mean follow up was 48 months (24-72). The clinical results were evaluated using MacNab's criteria.
RESULTS
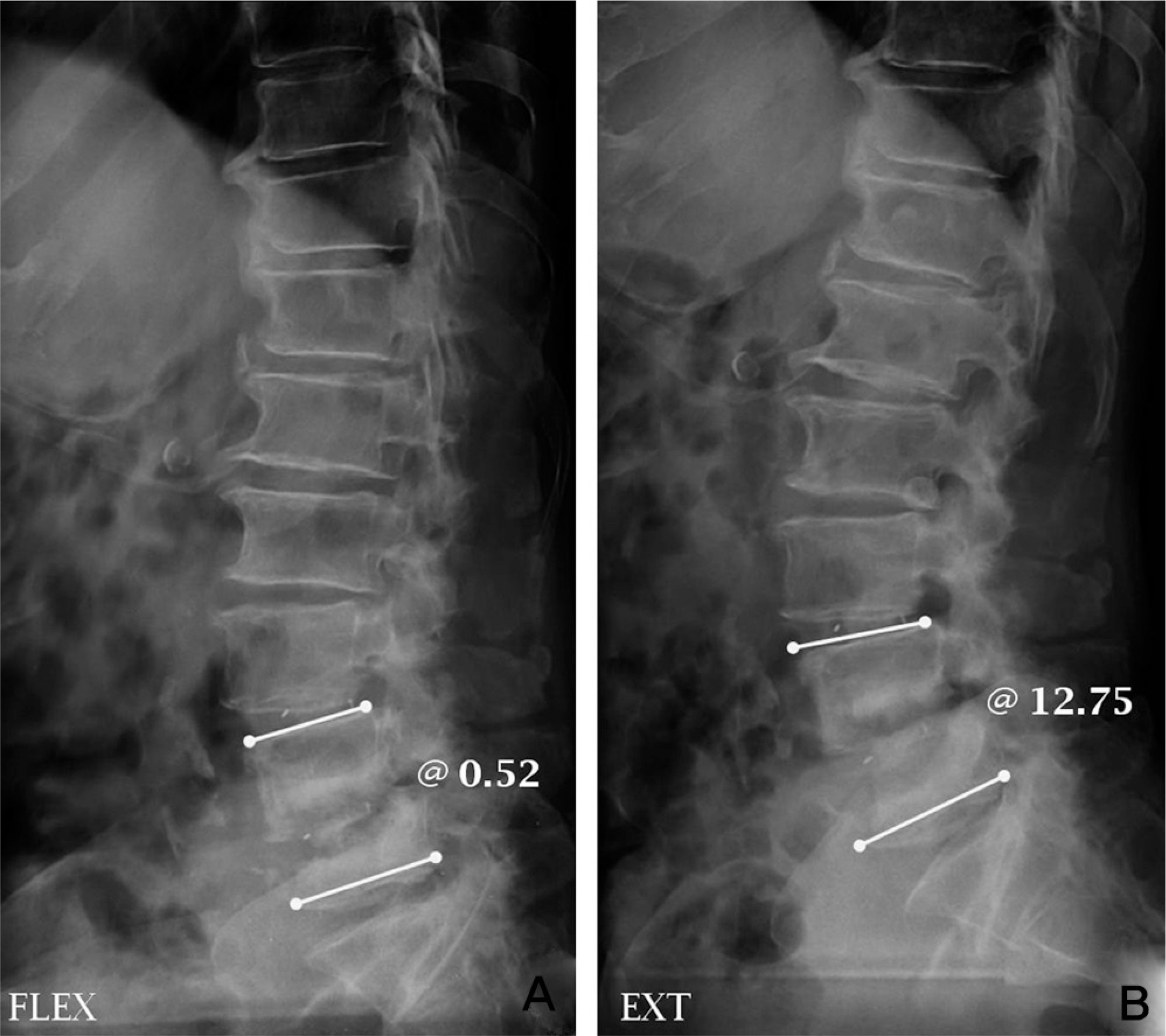
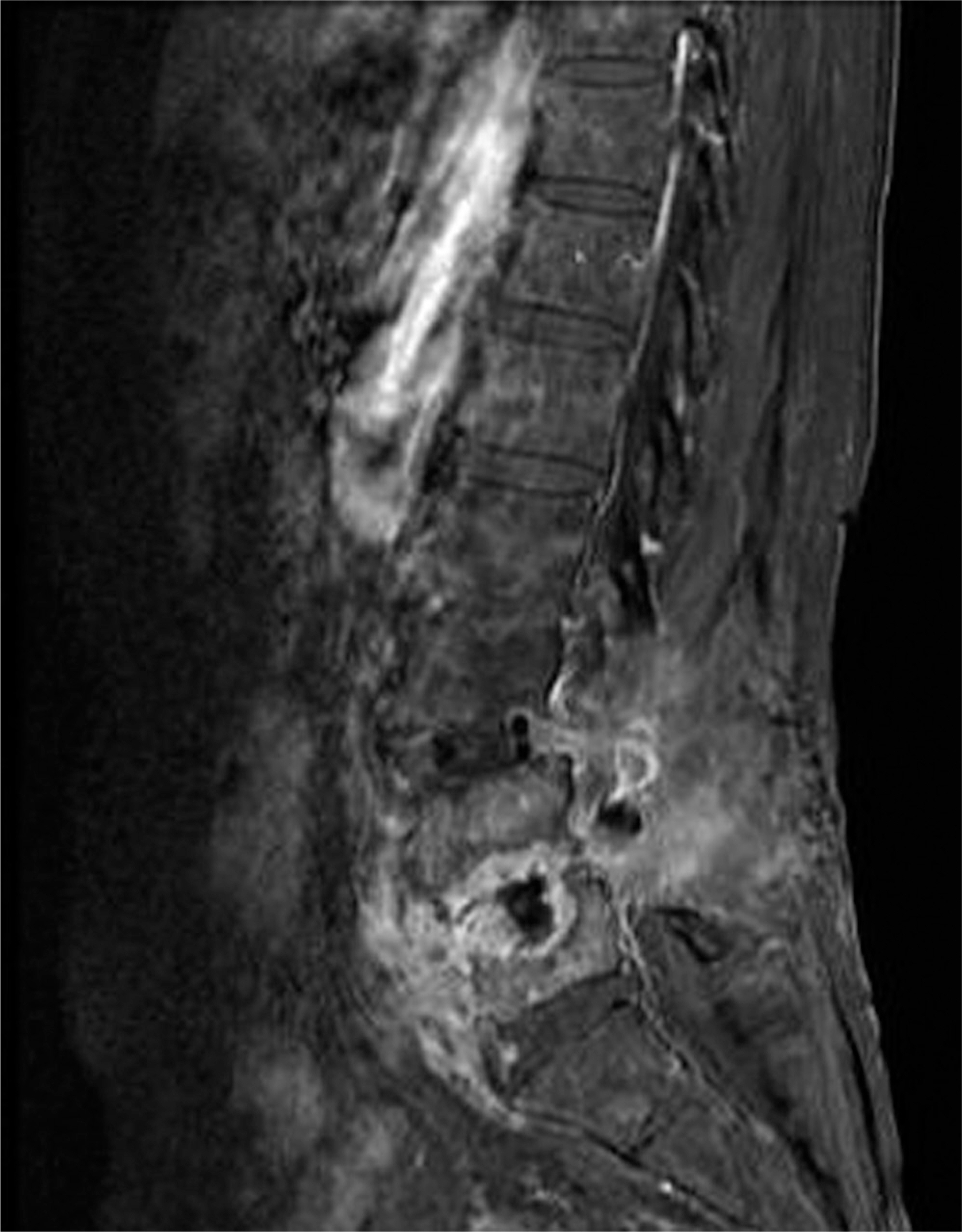
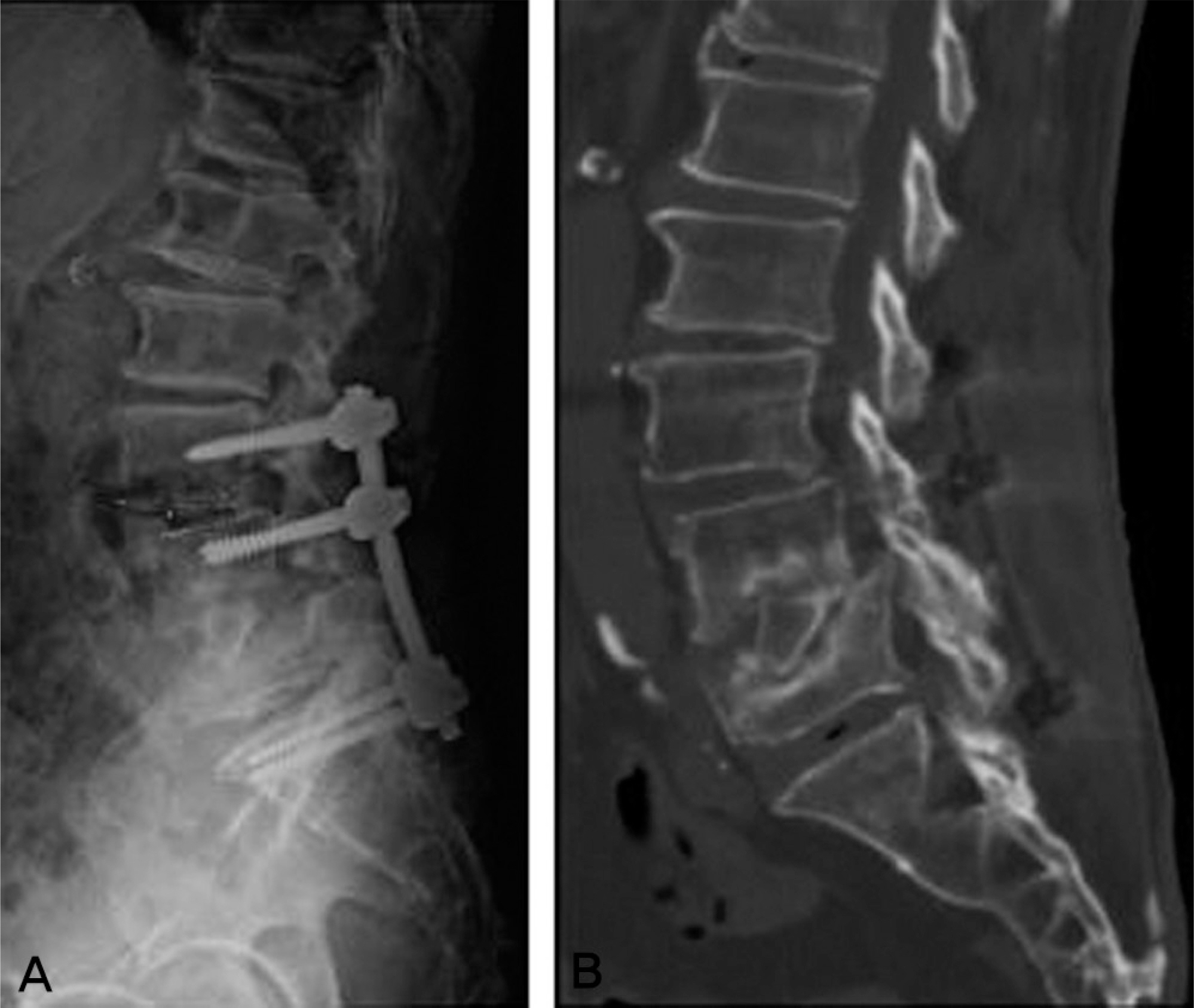
The diagnosis of infection was made based on the clinical symptoms and signs, and inflammatory markers, such as ESR and CRP. The time to diagnosis was less than one week (2), three weeks (2), six weeks (1) and three months or more (4). Bacterial identification was performed on seven cases. MRSA was detected in one of them, and no bacteria were identified in the other six. In two of them, the infection subsided with antibiotic therapy only. In 7 cases, removal of the cage and anterior iliac strut graft was needed for infection control. In four cases, loosened screws were removed during debridement. In 2 cases, additional surgery for pseudarthrosis was required after curing the infection.
CONCLUSIONS
In deep infections after PLIF, early diagnosis and bacterial identification are important for reducing the need for a later radical operation. It is recommended that blood markers of infection be measured with a short follow-up period. In a case of persistent infection against prolonged antibiotics, removal of the cage or screw is needed to treat the infection earlier.
MeSH Terms
Figure
Reference
-
1.Kuslich SD., Danielson G., Dowdle JD, et al. Four-year follow-up rusults of lumbar spine arthrodesis using Bagdy and Kuslich lumbar fusion cage. Spine. 2000. 25:2656–62.2.McAfee PC., Cunningham BW., Lee GY, et al. Revision strategies for salvaging or improving failed cylindrical cages. Spine. 1999. 24:2147–53.
Article3.Gertzbein SD., Betz R., Clements D, et al. Semirigid instrumentation in the management of lumbar spinal conditions combined with circumferential fusion. A multicenter study. Spine. 1996. 21:1918–25.4.Okuyama K., Abe E., Suzuki T, et al. Posterior lumbar interbody fusion: a retrospective study of complications after facet joint excision and pedicle screw fixation in 148 cases. Acta Orthop Scand. 1999. 70:329–34.
Article5.Ha KY., Kim YH. Postoperative spondylitis after posterior lumbar interbody fusion using cages. Eur Spine J. 2004. 13:419–24.
Article6.Bernard L., Hoffmeyer P., Assal M, et al. Trends in the treatment of orthopaedic prosthetic infections. J Antimicrob Chemother. 2004. 53:127–9.
Article7.Segreti J., Nelson JA., Trenholme GM. Prolonged suppressive antibiotic therapy for infected orthopedic prostheses. Clin Infect Dis. 1998. 27:711–3.
Article8.Kim EH., Song IS. Deep Wound Infection after Lumbar Spine Fusion with Pedicular Screw Fixation. J Korean Soc Spine Surg. 2000. 7:535–43.9.Moe JH. Complication of scoliosis treatment. Clin Orthop. 1967. 53:21–30.10.Prothero SR., Parkes JC., Stinchfield FE. Complications after low back fusion in 1000 patients. J Bone Joint Surg Am. 1966. 48:57–65.11.Lonstein J., Winter R., Moe J, et al. Wound infection with Harrington instrumentation and spine fusion for scoliosis. Clin Orthop. 1973. 96:222–33.
Article12.Mehbod AA., Ogilvie JW., Pinto MR, et al. Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure. J Spinal Disord Tech. 2005. 18:14–7.13.Heller JG., Garfin SR. Postoperative infection of the spine. Semin Spine Surg. 1990. 2:268–82.14.Heller JG., Whitecloud TS., Butler JC, et al. Complication of spinal surgery. Fothman RH, Simone FA, editors. The Spine. 3rd ed.Philadelphia: WB Saunders Company;1991. p. 1817–37.15.Jutte PC., Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002. 11:594–8.
Article16.Song KJ., Song KH., Park YK., Lee KB., Kim SL. Risk Factor of Deep Infection after Thoracic and Lumbar Spinal Arthrodesis. J Korean Soc Spine Surg. 2008. 15:149–54.17.Wimmer C., Gluch H. Management of post operative wound infection in posterior spinal fusion with instrumentation. J Spinal Disord. 1996. 9:505–8.18.Zucherman JF., Shaw SR., Hsu KY. Treatment of complications of BAK cages. Margulies JY, Aebi M, Farcy JP, editors. Revision Spine Surgery. St. Louis: Mosby;1999. p. 611.19.Mirovsky Y., Floman Y., Smorgick Y, et al. Management of Deep Wound infection After Posterior Lumbar Interbody Fusion With Cages. J Spinal Disord Tech. 2007. 20:127–31.
Article20.Glassman SD., Dimar JR., Puno RM., Johnson JR. Salvage of instrumented lumbar fusions complicated by surgical wound infection. Spine. 1996. 21:2163–9.
Article21.Levi AD., Dickman CA., Sonntag VK. Management of postoperative infection after spinal instrumentation. J Neurosurg. 1997. 86:975–80.22.Weinstein MA., McCabe JP., Cammisa FP. Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord. 2000. 13:422–6.
Article23.Richards BS. Delayed infectios following posterior spinal instrumentation for the treatment of idiopathic scoliosis. J Bone Joint Surg Am. 1995. 77:524–9.24.Theiss SM., Lonstein J., Winter R. Wound infections in reconstructive spine surgery. Orthop Clin North Am. 1996. 27:105–10.
Article25.Muschik M., Luck W., Schlenzka D. Implant removal for late-developing infection after instrumented posterior spinal fusion for scoliosis: re-instrumentation reduces loss of correction. A retrospective analysis of 45 cases. Eur Spine J. 2004. 13:645–51.
Article26.Collins I., Wilson-MacDonald J., Chami G, et al. The diagnosis and management of infection following instrumented spinal fusion. Eur Spine J. 2008. 17:445–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Future Development of Interbody Fusion Cages
- Management of Deep Wound Infection After Posterior Lumbar Interbody Fusion With Cages
- A novel technique for posterior lumbar interbody fusion to obtain a good local lordosis angle: anterior-release posterior lumbar interbody fusion
- Polyetheretherketone Versus Titanium Cages for Posterior Lumbar Interbody Fusion: Meta-Analysis and Review of the Literature
- Wedge Shape Cage in Posterior Lumbar Interbody Fusion: Focusing on Changes of Lordotic Curve