Clin Orthop Surg.
2011 Mar;3(1):55-61. 10.4055/cios.2011.3.1.55.
Effectiveness of Subacromial Anti-Adhesive Agent Injection after Arthroscopic Rotator Cuff Repair: Prospective Randomized Comparison Study
- Affiliations
-
- 1Department of Orthopedic Surgery, S-Seoul Hospital, Suwon, Korea.
- 2Department of Orthopaedic Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. doctoryub@naver.com
- 3Department of Orthopedic Surgery, Seoul Medical Center, Seoul, Korea.
- KMID: 999461
- DOI: http://doi.org/10.4055/cios.2011.3.1.55
Abstract
- BACKGROUND
Arthroscopic rotator cuff repair generally has a good clinical outcome but shoulder stiffness after surgery due to subacromial adhesion is one of the most common and clinically important complications. Sodium hyaluronate (HA) has been reported to be an anti-adhesive agent in a range of surgical procedures. However, there are few reports of the outcomes of arthroscopic rotator cuff repair of the shoulder. This study examined whether a subacromial injection of HA/carboxymethylated cellulose (CMC) affected the postoperative shoulder stiffness and healing of rotator cuff repair, as well as the safety of an injection.
METHODS
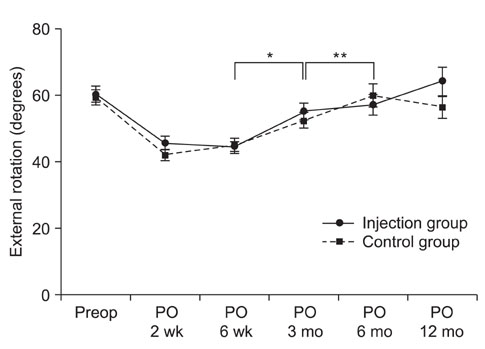
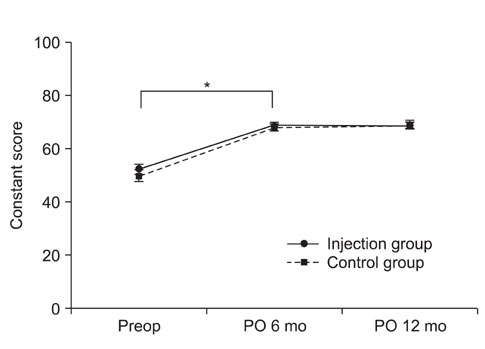
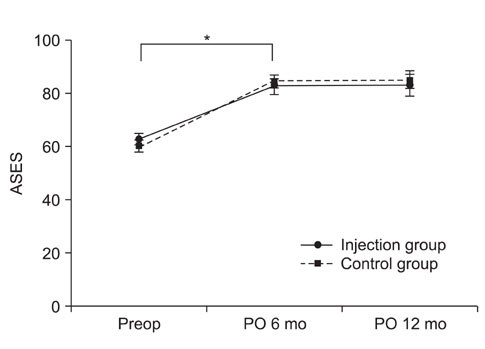
Between January 2008 and May 2008, 80 consecutive patients with arthroscopic rotator cuff repair were enrolled. The patients were assigned randomly to the HA/CMC injection group (n = 40) or control group (n = 40). All patients were evaluated using the visual analog scale (VAS) for pain, passive range of motion at 2, 6 weeks, 3, 6, 12 months after surgery, and the functional scores at 6, 12 months postoperatively. Cuff healing was also evaluated using CT arthrography or ultrasonography at 6 or 12 months after surgery.
RESULTS
The HA/CMC injection group showed faster recovery of forward flexion at 2 weeks postoperatively than the control group but the difference was not statistically significant (p = 0.09). There were no significant difference in pain VAS, internal rotation, external rotation and functional scores between two groups at each follow-up period. The functional scores improved 6 months after surgery in both groups but there were no differences between the two groups. The incidence of unhealed rotator cuff was similar in the two groups. There were no complications related to an injection of anti-adhesive agents including wound problems or infections.
CONCLUSIONS
A subacromial injection of an anti-adhesive agent after arthroscopic rotator cuff repair tended to produce faster recovery in forward flexion with no adverse effects on cuff healing. However, its anti-adhesive effects after rotator cuff repair should be considered carefully with further studies.
MeSH Terms
-
Adult
Aged
Arthroscopy/*adverse effects/*methods
Carboxymethylcellulose Sodium
Drug Carriers
Female
Humans
Hyaluronic Acid/adverse effects/*therapeutic use
Male
Middle Aged
Pain
Prospective Studies
Range of Motion, Articular
Recovery of Function
Rotator Cuff/injuries/*surgery
Shoulder Joint/physiology
Tissue Adhesions/*prevention & control
Treatment Outcome
Viscosupplements/adverse effects/*therapeutic use
Figure
Cited by 3 articles
-
Pharmacologic treatment of osteoarthritis
Seung-Hoon Baek, Shin-Yoon Kim
J Korean Med Assoc. 2013;56(12):1123-1131. doi: 10.5124/jkma.2013.56.12.1123.What Do the Patients Want and Worry in Korean Patients Who Undergo Arthroscopic Rotator Cuff Surgery?
Jong Pil Yoon, Joo Han Oh, Woo-Kie Min, Joon Woo Kim, Won-Ju Jeong, Hyun-Joo Lee
Clin Orthop Surg. 2012;4(4):278-283. doi: 10.4055/cios.2012.4.4.278.What Do the Patients Want and Worry in Korean Patients Who Undergo Arthroscopic Rotator Cuff Surgery?
Jong Pil Yoon, Joo Han Oh, Woo-Kie Min, Joon Woo Kim, Won-Ju Jeong, Hyun-Joo Lee
Clin Orthop Surg. 2012;4(4):278-283. doi: 10.4055/cios.2012.4.4.278.
Reference
-
1. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004. 86(2):219–224.
Article2. Nho SJ, Adler RS, Tomlinson DP, et al. Arthroscopic rotator cuff repair: prospective evaluation with sequential ultrasonography. Am J Sports Med. 2009. 37(10):1938–1945.3. Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007. 23(2):124–128.
Article4. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009. 25(8):880–890.
Article5. Hagberg L, Gerdin B. Sodium hyaluronate as an adjunct in adhesion prevention after flexor tendon surgery in rabbits. J Hand Surg Am. 1992. 17(5):935–941.
Article6. Tuncay I, Ozbek H, Atik B, Ozen S, Akpinar F. Effects of hyaluronic acid on postoperative adhesion of tendo calcaneus surgery: an experimental study in rats. J Foot Ankle Surg. 2002. 41(2):104–108.
Article7. Fujii S, Shimada H, Ike H, et al. Reduction of postoperative abdominal adhesion and ileus by a bioresorbable membrane. Hepatogastroenterology. 2009. 56(91-92):725–728.8. Mais V, Bracco GL, Litta P, Gargiulo T, Melis GB. Reduction of postoperative adhesions with an auto-crosslinked hyaluronan gel in gynaecological laparoscopic surgery: a blinded, controlled, randomized, multicentre study. Hum Reprod. 2006. 21(5):1248–1254.
Article9. Kato T, Haro H, Komori H, Shinomiya K. Evaluation of hyaluronic acid sheet for the prevention of postlaminectomy adhesions. Spine J. 2005. 5(5):479–488.
Article10. Akeson WH, Massie JB, Huang B, et al. Topical high-molecular-weight hyaluronan and a roofing barrier sheet equally inhibit postlaminectomy fibrosis. Spine J. 2005. 5(2):180–190.
Article11. Shimpuku E, Hamada K, Handa A, et al. Molecular effects of sodium hyaluronate on the healing of avian supracoracoid tendon tear: according to in situ hybridization and real-time polymerase chain reaction. J Orthop Res. 2007. 25(2):173–184.
Article12. Yamada T, Gotoh M, Nakama K, Mitsui Y, Higuchi F, Nagata K. Effects of hyaluronan on cell proliferation and mRNA expression of procollagens alpha 1 (I) and alpha 1 (III) in tendon-derived fibroblasts from patients with rotator cuff disease: an in vitro study. Am J Sports Med. 2007. 35(11):1870–1876.
Article13. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008. 24(9):983–991.
Article14. Iocono JA, Ehrlich HP, Keefer KA, Krummel TM. Hyaluronan induces scarless repair in mouse limb organ culture. J Pediatr Surg. 1998. 33(4):564–567.
Article15. Stern M, Longaker MT, Stern R. Adzick NS, Longaker MT, editors. Hyaluronic acid and its modulation in fetal and adult wound healing. Fetal wound healing. 1991. New York: Elsevier;189–198.16. Ferguson MW. Skin wound healing: transforming growth factor beta antagonists decrease scarring and improve quality. J Interferon Res. 1994. 14(5):303–304.
Article17. Shah M, Whitby DJ, Ferguson MW. Jackson IT, Sommerlad BC, editors. Fetal wound healing and scarless surgery. Recent advances in plastic surgery. 1996. Edinburgh: Churchill Livingstone.18. Kumar S, Wong PF, Leaper DJ. Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev. 2009. (1):CD005080.
Article19. Liu Y, Skardal A, Shu XZ, Prestwich GD. Prevention of peritendinous adhesions using a hyaluronan-derived hydrogel film following partial-thickness flexor tendon injury. J Orthop Res. 2008. 26(4):562–569.
Article20. Menderes A, Mola F, Tayfur V, Vayvada H, Barutcu A. Prevention of peritendinous adhesions following flexor tendon injury with seprafilm. Ann Plast Surg. 2004. 53(6):560–564.
Article21. Shibata Y, Midorikawa K, Emoto G, Naito M. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Shoulder Elbow Surg. 2001. 10(3):209–216.
Article22. Moskowitz RW, Blaine TA. An overview of treatment options for persistent shoulder pain. Am J Orthop (Belle Mead NJ). 2005. 34:12 Suppl. 10–15.23. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005. 87(6):1229–1240.
Article24. Trenerry K, Walton JR, Murrell GA. Prevention of shoulder stiffness after rotator cuff repair. Clin Orthop Relat Res. 2005. (430):94–99.
Article25. Rockwood CA Jr, Matsen FA 3rd, Wirth MA, Lippitt SB, Fehringer EV, Sperling JW. The shoulder. 2009. 4th ed. Philadelphia: Saunders;899–902.26. Brecht M, Mayer U, Schlosser E, Prehm P. Increased hyaluronate synthesis is required for fibroblast detachment and mitosis. Biochem J. 1986. 239(2):445–450.
Article27. Chen WY, Abatangelo G. Functions of hyaluronan in wound repair. Wound Repair Regen. 1999. 7(2):79–89.
Article28. de Wit T, de Putter D, Tra WM, et al. Auto-crosslinked hyaluronic acid gel accelerates healing of rabbit flexor tendons in vivo. J Orthop Res. 2009. 27(3):408–415.
Article29. Strickland JW. Development of flexor tendon surgery: twenty-five years of progress. J Hand Surg Am. 2000. 25(2):214–235.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revisional Rotator Cuff Repair
- Effectiveness of the Anti-adhesive Agent Protescal after Arthroscopic Rotator Cuff Repair: A Retrospective Study
- Efficacy and Safety of Combined Subacromial and Intravenous Patient-controlled Analgesia after Arthroscopic Rotator Cuff Repair
- Rotator Cuff Repair using Mini - open Technique with Minimized Arthroscopic Acromioplasty
- Can It be Said that this Case Confirmed the Phenomenon of Subacromial Suture Knot Impingement after Arthroscopic Rotator Cuff Repair?: A Case Report