Clin Orthop Surg.
2010 Sep;2(3):140-147. 10.4055/cios.2010.2.3.140.
Survival and Prognostic Analysis of Adjacent Segments after Spinal Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea. hoon0319@gmail.com
- KMID: 999432
- DOI: http://doi.org/10.4055/cios.2010.2.3.140
Abstract
- BACKGROUND
To examine the survival function and prognostic factors of the adjacent segments based on a second operation after thoracolumbar spinal fusion.
METHODS
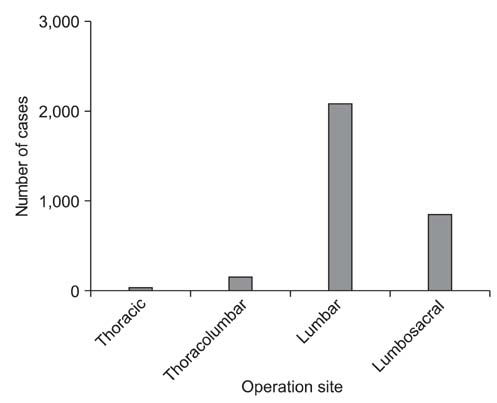
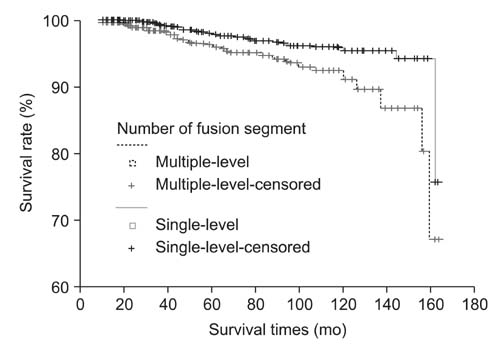
This retrospective study reviewed 3,188 patients (3,193 cases) who underwent a thoracolumbar spinal fusion at the author's hospital. Survival analysis was performed on the event of a second operation due to adjacent segment degeneration. The prognostic factors, such as the cause of the disease, surgical procedure, age, gender and number of fusion segments, were examined. Sagittal alignment and the location of the adjacent segment were measured in the second operation cases, and their association with the types of degeneration was investigated.
RESULTS
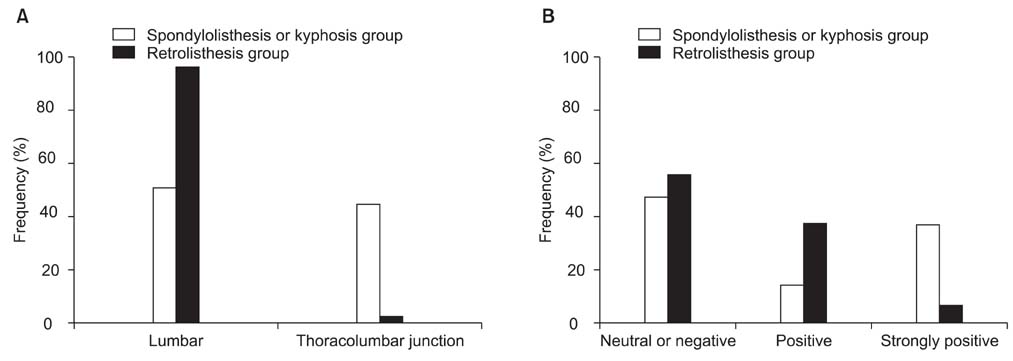
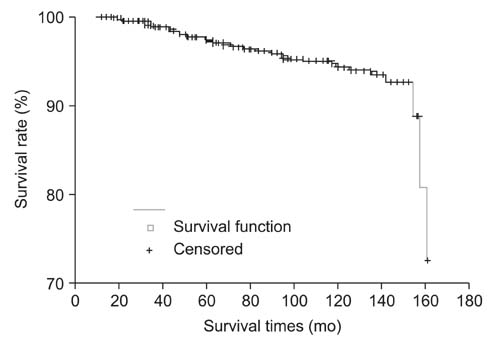
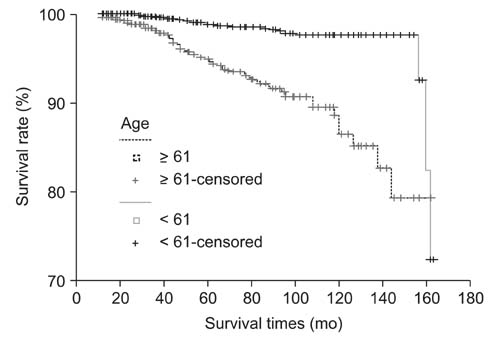
One hundred seven patients, 112 cases (3.5%), underwent a second operation due to adjacent segment degeneration. The survival function was 97% and 94% at 5 and 10 years after surgery, respectively, showing a 0.6% linear reduction per year. The significant prognostic factors were old age, degenerative disease, multiple-level fusion and male. Among the second operation cases, the locations of the adjacent segments were the thoracolumbar junctional area and lumbosacral area in 11.6% and 88.4% of cases, respectively. Sagittal alignment was negative or neutral, positive and strongly positive in 47.3%, 38.9%, and 15.7%, respectively. Regarding the type of degeneration, spondylolisthesis or kyphosis, retrolisthesis, and neutral balance in the sagittal view was noted in 13.4%, 36.6%, and 50% of cases, respectively. There was a significant difference according to the location of the adjacent segment (p = 0.000) and sagittal alignment (p = 0.041).
CONCLUSIONS
The survival function of the adjacent segments was 94% at 10 years, which had decreased linearly by 0.6% per a year. The likelihood of a second operation was high in those with old age, degenerative disease, multiple-level fusion and male. There was a tendency for the type of degeneration to be spondylolisthesis or kyphosis in cases of the thoracolumbar junctional area and strongly positive sagittal alignment, but retrolisthesis in cases of the lumbosacral area and neutral or positive sagittal alignment.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Lumbosacral Fixation Using the Diagonal S2 Screw for Long Fusion in Degenerative Lumbar Deformity: Technical Note Involving 13 Cases
Ye-Soo Park, Hong-Sik Kim, Seung-Wook Baek, Sang-Hyun Lee
Clin Orthop Surg. 2013;5(3):225-229. doi: 10.4055/cios.2013.5.3.225.Survival Rates and Risk Factors for Cephalad and L5-S1 Adjacent Segment Degeneration after L5 Floating Lumbar Fusion : A Minimum 2-Year Follow-Up
Young-Seok Lee, Young-Baeg Kim, Seung-Won Park
J Korean Neurosurg Soc. 2015;57(2):108-113. doi: 10.3340/jkns.2015.57.2.108.
Reference
-
1. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991. 73(6):802–808.
Article2. Mardjetko SM, Connolly PJ, Shott S. Degenerative lumbar spondylolisthesis: a meta-analysis of literature 1970-1993. Spine (Phila Pa 1976). 1994. 19:Suppl 20. 2256S–2265S.3. Highsmith JM, Tumialan LM, Rodts GE Jr. Flexible rods and the case for dynamic stabilization. Neurosurg Focus. 2007. 22(1):E11.4. Beastall J, Karadimas E, Siddiqui M, et al. The Dynesys lumbar spinal stabilization system: a preliminary report on positional magnetic resonance imaging findings. Spine (Phila Pa 1976). 2007. 32(6):685–690.5. Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976). 2008. 33(15):1701–1707.
Article6. Kulkarni AG, Diwan AD. Prosthetic lumbar disc replacement for degenerative disc disease. Neurol India. 2005. 53(4):499–505.
Article7. Bothmann M, Kast E, Boldt GJ, Oberle J. Dynesys fixation for lumbar spine degeneration. Neurosurg Rev. 2008. 31(2):189–196.8. Lee S, Ahn DK, Jeong KW, Kim HS, Seo YH, Park HS. Altered sagittal rotation after segmental fusion in degenerative lumbar disease: comparative study by level, length of fused segments. J Korean Soc Spine Surg. 2004. 11(4):231–237.
Article9. Axelsson P, Johnsson R, Stromqvist B. Adjacent segment hypermobility after lumbar spine fusion: no association with progressive degeneration of the segment 5 years after surgery. Acta Orthop. 2007. 78(6):834–839.
Article10. Hoogendoorn RJ, Helder MN, Wuisman PI, Bank RA, Everts VE, Smit TH. Adjacent segment degeneration: observations in a goat spinal fusion study. Spine (Phila Pa 1976). 2008. 33(12):1337–1343.11. Ahn DK, Lee S, Jeong KW, Park JS, Cha SK, Park HS. Adjacent segment failure after lumbar spine fusion: controlled study for risk factors. J Korean Orthop Assoc. 2005. 40(2):203–208.
Article12. Eck JC, Humphreys SC, Hodges SD. Adjacent-segment degeneration after lumbar fusion: a review of clinical, biomechanical, and radiologic studies. Am J Orthop (Belle Mead NJ). 1999. 28(6):336–340.13. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:2 Suppl. 163–169.
Article14. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004. 86(7):1497–1503.
Article15. Hayashi T, Arizono T, Fujimoto T, et al. Degenerative change in the adjacent segments to the fusion site after posterolateral lumbar fusion with pedicle screw instrumentation: a minimum 4-year follow-up. Fukuoka Igaku Zasshi. 2008. 99(5):107–113.16. Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987. 12(2):97–104.
Article17. Min JH, Jang JS, Jung B, et al. The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech. 2008. 21(5):305–309.
Article18. Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976). 2004. 29(14):1535–1540.
Article19. Wiltse LL, Radecki SE, Biel HM, et al. Comparative study of the incidence and severity of degenerative change in the transition zones after instrumented versus noninstrumented fusions of the lumbar spine. J Spinal Disord. 1999. 12(1):27–33.
Article20. Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005. 10(5):490–495.
Article21. Throckmorton TW, Hilibrand AS, Mencio GA, Hodge A, Spengler DM. The impact of adjacent level disc degeneration on health status outcomes following lumbar fusion. Spine (Phila Pa 1976). 2003. 28(22):2546–2550.
Article22. Ha KY, Kim KW, Park SJ, Lee YH. Changes of the adjacent-unfused mobile segment after instrumental lumbar fusion: more than 5-years follow-up. J Korean Soc Spine Surg. 1998. 5(2):205–214.23. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995. 8(6):464–473.
Article24. Bastian L, Lange U, Knop C, Tusch G, Blauth M. Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J. 2001. 10(4):295–300.
Article25. Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976). 1998. 23(14):1550–1558.
Article26. Weinhoffer SL, Guyer RD, Herbert M, Griffith SL. Intradiscal pressure measurements above an instrumented fusion: a cadaveric study. Spine (Phila Pa 1976). 1995. 20(5):526–531.27. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 1996. 9(5):392–400.28. Ahn DK, Lee S, Jeong KW, Choi DJ, Cha SK, Cho KH. Degenerative change of adjacent segments according to the fusion method after L4-5 segmental fusion: comparative study of posterolateral fusion and posterior lumbar interbody fusion. J Korean Orthop Assoc. 2006. 41(2):281–287.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence And Risk Factor of Degenerative Disease of Adjacent Segment after Anterior Cervical Arthrodesis
- Survival Rates and Risk Factors for Cephalad and L5-S1 Adjacent Segment Degeneration after L5 Floating Lumbar Fusion : A Minimum 2-Year Follow-Up
- Changes of the Adjacent Mobile Segment After Cat Spine Fixation
- Association between ligamentous stenosis at spondylolisthetic segments before fusion surgery and symptomatic adjacent canal stenosis at follow-up in patients with degenerative spondylolisthesis
- The Changes of Adjacent Segments after Spinal Fusion: Follow-up more than Three Years after Spinal Fusion