Korean J Radiol.
2010 Jun;11(3):312-319. 10.3348/kjr.2010.11.3.312.
Embolotherapy for Pulmonary Arteriovenous Malformations in Patients without Hereditary Hemorrhagic Telangiectasia
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 138-736, Korea. jhshin@amc.seoul.kr
- KMID: 946271
- DOI: http://doi.org/10.3348/kjr.2010.11.3.312
Abstract
OBJECTIVE
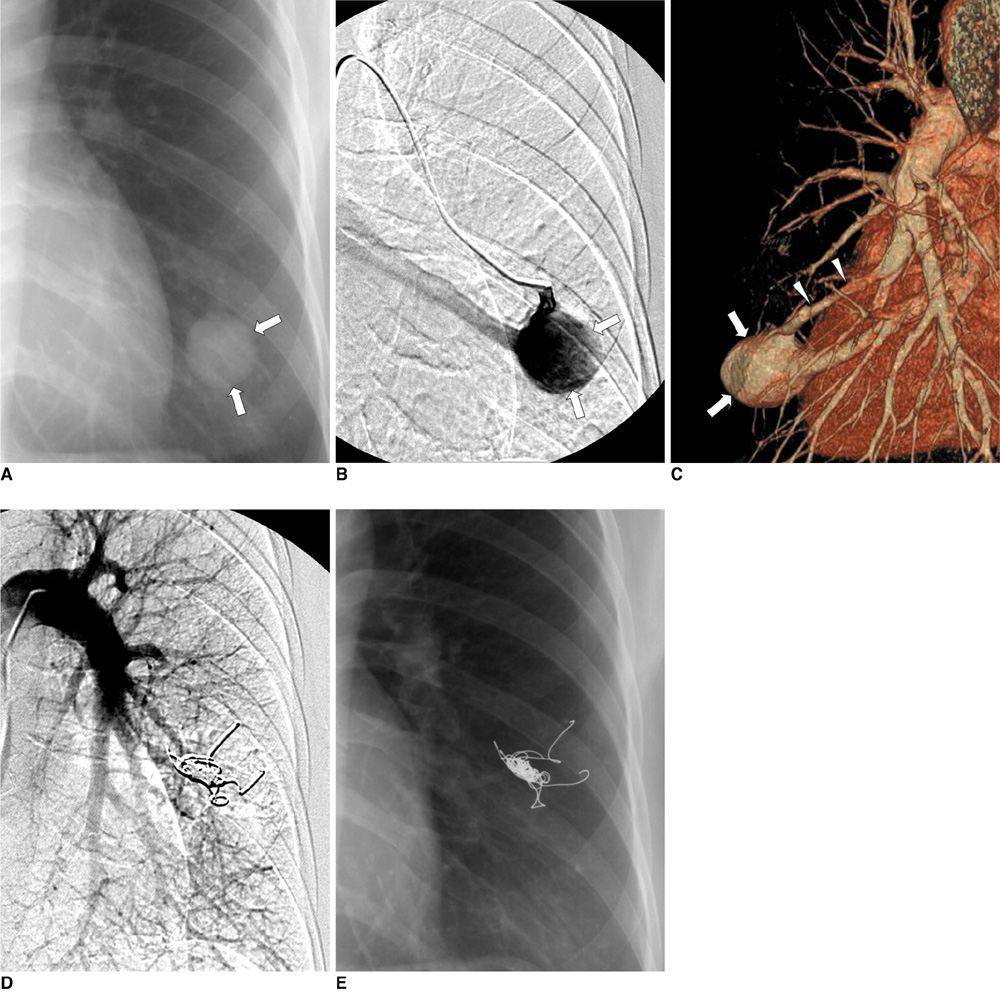
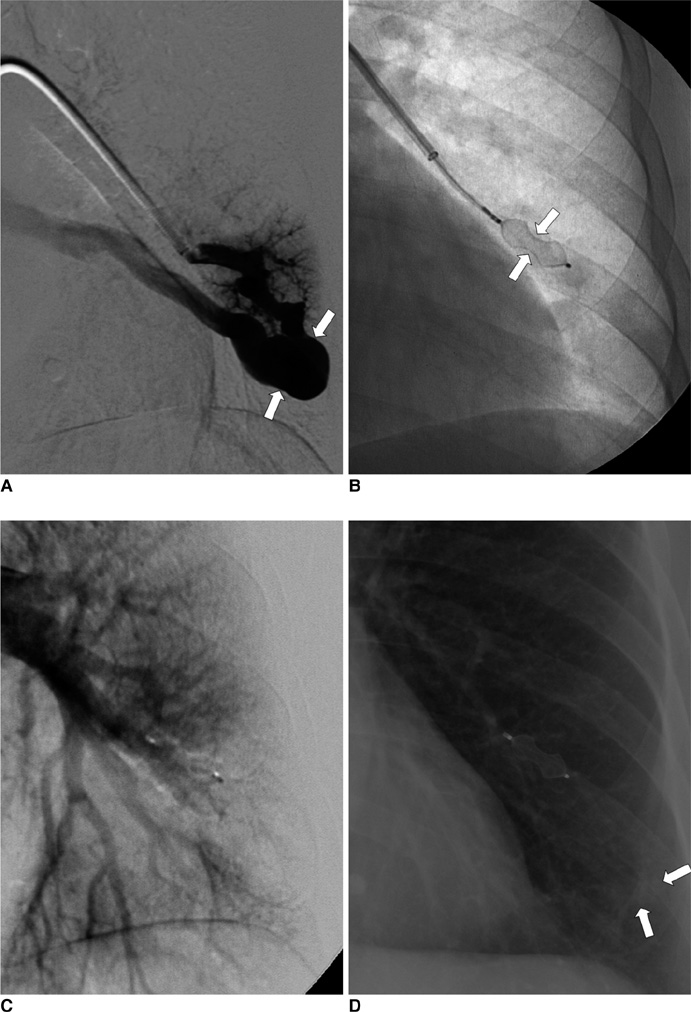
To evaluate the clinical and radiological outcomes of transcatheter embolotherapy for treating sporadic pulmonary arteriovenous malformations (PAVMs) that were not associated with hereditary hemorrhagic telangiectasia. MATERIALS AND METHODS: Between January 2001 and June 2008, thirty-five sporadic PAVMs were detected in 23 patients. The clinical follow up consisted of assessing the changes of the signs and symptoms of the PAVMs, and radiological evaluation with chest radiographs or chest CT scans. RESULTS: The lower lung regions (63%) and peripheral locations (86%) were the common locations of the PAVMs. Thirty-four PAVMs (97%) had simple architecture (one arterial feeder within a single pulmonary segment). Technical success was achieved in 33 PAVMs (94%); two cases of technical failure were due to catheterization failure (n = 1) and too large a feeding artery (17 mm) that disabled embolotherapy (n = 1). Coils and Amplatz vascular plugs were used in 30 and three PAVMs, respectively. Inadvertent placement of one coil (n = 1) and pulmonary infarction (n = 1) occurred, but no relevant symptoms developed. For the 13 patients with available data, the mean arterial O2 saturation changed significantly from 92% to 98%. Complete or near-complete involution of the sac was observed in 30 of the 33 embolized PAVMs (91%). In these 33 embolized PAVMs, the mean sac diameter significantly decreased from 17.83 mm to 0.68 mm. CONCLUSION: Sporadic PAVMs are mostly the simple type with predominance in the lower lobe and peripheral locations. Transcatheter embolotherapy with coils or Amplatz vascular plugs is a safe and effective treatment for sporadic PAVMs and this provides excellent functional and radiological improvement.
Keyword
MeSH Terms
-
Adolescent
Adult
Aged
Arteriovenous Malformations/radiography/*therapy
Child
Cohort Studies
Embolization, Therapeutic/*methods
Female
Humans
Male
Middle Aged
Pulmonary Artery/*radiography
Pulmonary Veins/*radiography
*Telangiectasia, Hereditary Hemorrhagic
Tomography, X-Ray Computed/methods
Treatment Outcome
Young Adult
Figure
Reference
-
1. Cottin V, Plauchu H, Bayle JY, Barthelet M, Revel D, Cordier JF. Pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Am J Respir Crit Care Med. 2004. 169:994–1000.2. White RI Jr, Pollak JS, Wirth JA. Pulmonary arteriovenous malformations: diagnosis and transcatheter embolotherapy. J Vasc Interv Radiol. 1996. 7:787–804.3. Cottin V, Chinet T, Lavolé A, Corre R, Marchand E, Reynaud-Gaubert M, et al. Pulmonary arteriovenous malformations in hereditary hemorrhagic telangiectasia: a series of 126 patients. Medicine (Baltimore. 2007. 86:1–17.4. Gupta P, Mordin C, Curtis J, Hughes JM, Shovlin CL, Jackson JE. Pulmonary arteriovenous malformations: effect of embolization on right-to-left shunt, hypoxemia, and exercise tolerance in 66 patients. AJR Am J Roentgenol. 2002. 179:347–355.5. Mager JJ, Overtoom TT, Blauw H, Lammers JW, Westermann CJ. Embolotherapy of pulmonary arteriovenous malformations: long-term results in 112 patients. J Vasc Interv Radiol. 2004. 15:451–456.6. Pollak JS, Saluja S, Thabet A, Henderson KJ, Denbow N, White RI Jr. Clinical and anatomic outcomes after embolotherapy of pulmonary arteriovenous malformations. J Vasc Interv Radiol. 2006. 17:35–44.7. Swanson KL, Prakash UB, Stanson AW. Pulmonary arteriovenous fistulas: Mayo Clinic experience, 1982-1997. Mayo Clin Proc. 1999. 74:671–680.8. Shovlin CL, Guttmacher AE, Buscarini E, Faughnan ME, Hyland RH, Westermann CJ, et al. Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet. 2000. 91:66–67.9. Remy-Jardin M, Dumont P, Brillet PY, Dupuis P, Duhamel A, Remy J. Pulmonary arteriovenous malformations treated with embolotherapy: helical CT evaluation of long-term effectiveness after 2-21-year follow-up. Radiology. 2006. 239:576–585.10. Pierucci P, Murphy J, Henderson KJ, Chyun DA, White RI Jr. New definition and natural history of patients with diffuse pulmonary arteriovenous malformations: twenty-seven-year experience. Chest. 2008. 133:653–661.11. White RI Jr, Lynch-Nyhan A, Terry P, Buescher PC, Farmlett EJ, Charnas L, et al. Pulmonary arteriovenous malformations: techniques and long-term outcome of embolotherapy. Radiology. 1988. 169:663–669.12. Dines DE, Arms RA, Bernatz PE, Gomes MR. Pulmonary arteriovenous fistulas. Mayo Clinic Proc. 1974. 49:460–465.13. Moussouttas M, Fayad P, Rosenblatt M, Hashimoto M, Pollak J, Henderson K, et al. Pulmonary arteriovenous malformations: cerebral ischemia and neurologic manifestations. Neurology. 2000. 55:959–964.14. Andersen PE, Kjeldsen AD. Occlusion of pulmonary arteriovenous malformations by use of vascular plug. Acta Radiol. 2007. 48:496–499.15. Ferro C, Rossi UG, Bovio G, Seitun S, Rossi GA. Percutaneous transcatheter embolization of a large pulmonary arteriovenous fistula with an amplatzer vascular plug. Cardiovasc Intervent Radiol. 2007. 30:328–331.16. Prasad V, Chan RP, Faughnan ME. Embolotherapy of pulmonary arteriovenous malformations: efficacy of platinum versus stainless steel coils. J Vasc Interv Radiol. 2004. 15:153–160.17. Haitjema T, ten Berg JM, Overtoom TT, Ernst JM, Westermann CJ. Unusual complications after embolization of a pulmonary arteriovenous malformation. Chest. 1996. 109:1401–1404.18. Brillet PY, Dumont P, Bouaziz N, Duhamel A, Laurent F, Remy J, et al. Pulmonary arteriovenous malformation treated with embolotherapy: systemic collateral supply at multidetector CT angiography after 2-20-year follow-up. Radiology. 2007. 242:267–276.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hereditary Hemorrhagic Telangiectasia Combined with Pulmonary Arteriovenous Malformation Treated with Transcatheter Embolotherapy
- Cerebral Infarction after Embolization for Pulmonary Arteriovenous Malformation in a Patient with Hereditary Hemorrhagic Telangiectasia
- A Case of Hepatic Involvement in Hereditary Hemorrhagic Telangiectasia Presenting as High Output Heart Failure
- A Case of Hereditary Hemorrhagic Telangiectasia
- A case of hereditary hemorrhagic telangiectasia