Korean J Lab Med.
2008 Jun;28(3):196-200. 10.3343/kjlm.2008.28.3.196.
Acute Lymphadenitis with Cellulitis Caused by Staphylococcus lugdunensis
- Affiliations
-
- 1Department of Laboratory Medicine, College of Medicine, Inje University, Busan, Korea. jhsmile@inje.ac.kr
- 2Department of Otolaryngology, College of Medicine, Inje University, Busan, Korea.
- 3Paik Institute for Clinical Research, College of Medicine, Inje University, Busan, Korea.
- 4Department of Nursing, Gwangju Health College, Gwangju, Korea.
- KMID: 854866
- DOI: http://doi.org/10.3343/kjlm.2008.28.3.196
Abstract
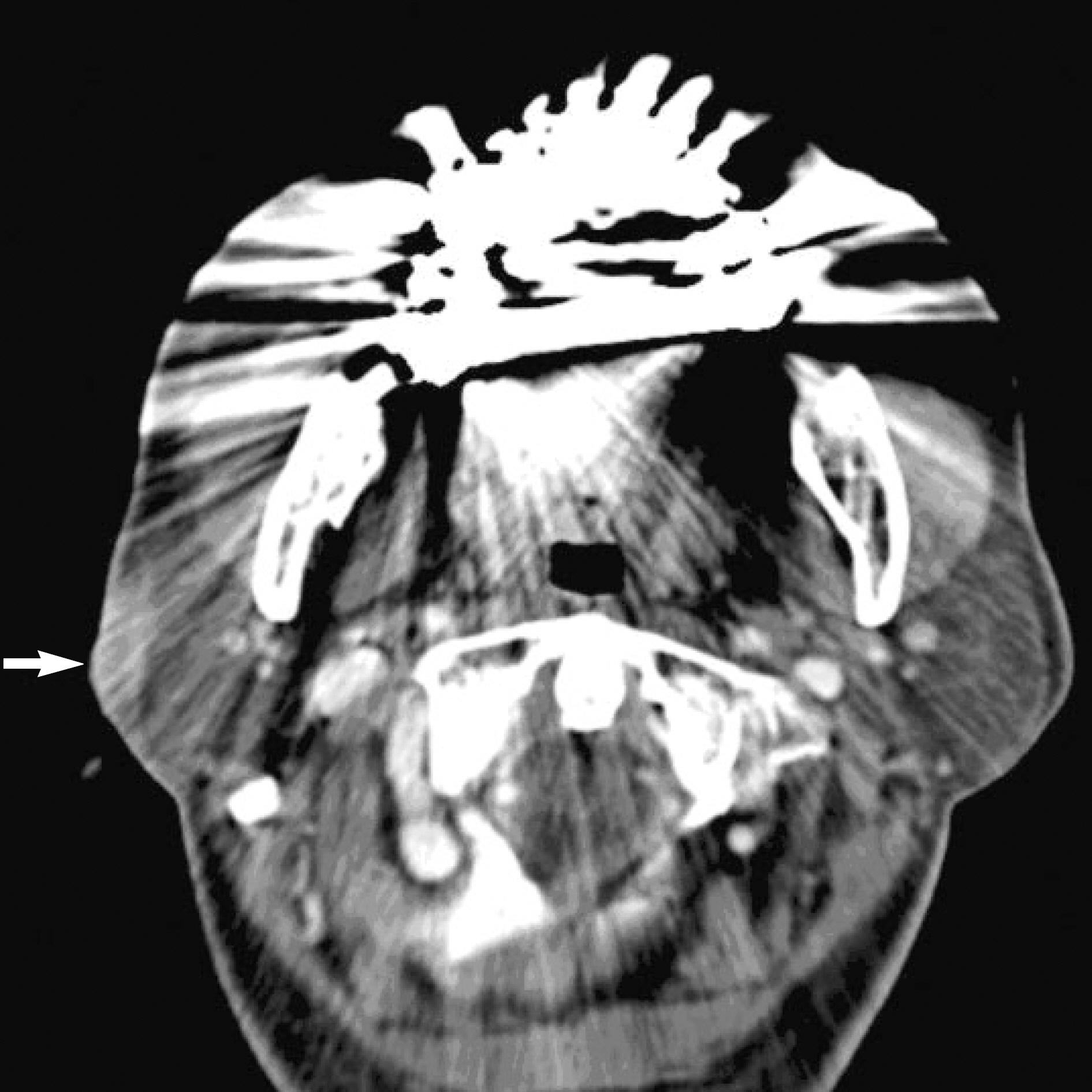
- Although coagulase-negative staphylococci (CNS) have been considered part of the resident flora on the human skin, Staphylococcus lugdunensis is an unusually virulent CNS and can cause many types of infection. We report a rare case of acute lymphadenitis with cellulitis in the right infraauricular region caused by S. lugdunensis. A 62-yr-old woman visited the Department of Otolaryngology of Busan Paik university hospital. She had a palpable mass and swelling in the right infraauricular region and complained of aggressive pain and a febrile sensation in the region for 5 days. On the suspicion of abscess with infection, percutaneous aspiration was performed and smooth, flat, white, opaque colonies grew on a blood agar plate as a pure culture. The biochemical test results showed the organism to be catalase positive, tube coagulase negative, ornithine decarboxylase positive, slide coagulase positive, and latex agglutination tests for coagulase positive. The API Staph Kit was used to identify the isolate to the species level as S. lugdunensis with a 64.6% probability (profile 6716152). We confirmed the species identification of this strain by 16S rDNA sequence analysis. The patient's clinical condition improved with appropriate antimicrobial therapy and pus drainage.
MeSH Terms
Figure
Cited by 1 articles
-
Streptococcus dysgalactiae subsp. equisimilis Possessing Lancefield's Group A Antigen
Jong Ae Son, Jeong Hwan Shin
Lab Med Online. 2013;3(1):60-61. doi: 10.3343/lmo.2013.3.1.60.
Reference
-
1.Freney J., Brun B., Bes M., Meugnier H., Grimont F., Grimont PAD, et al. Staphylococcus lugdunensis sp. nov. and Staphylococcus schleiferi sp. nov., two species from human clinical specimens. Int J Syst Bacteriol. 1988. 38:168–72.2.van der Mee-Marquet N., Achard A., Mereghetti L., Danton A., Minier M., Quentin R. Staphylococcus lugdunensis infections: high frequency of inguinal area carriage. J Clin Microbiol. 2003. 41:1404–9.3.Herchline TE., Ayers LW. Occurrence of Staphylococcus lugdunensis in consecutive clinical cultures and relationship of isolation to infection. J Clin Microbiol. 1991. 29:419–21.4.Patel R., Piper KE., Rouse MS., Uhl JR., Cockerill FR 3rd., Steckelberg JM. Frequency of isolation of Staphylococcus lugdunensis among staphylococcal isolates causing endocarditis: a 20-year experience. J Clin Microbiol. 2000. 38:4262–3.5.Kim KJ., Shin JH., Shin DH., Choi MJ., Cho D., Kee SJ, et al. Prevalence of pathogens causing central venous catheter (CVC)-related sepsis: results of semiquantitative CVC tip cultures and differential quantitative blood cultures. Korean J Lab Med. 2002. 22:260–6. (김광진, 신종희, 신동현, 채명종, 조덕, 기승정등. 중심정맥관Tip 배양과정량혈액배양을이용한중심정맥관관련패혈증의진단및원인균분석. 대한진단검사의학회지 2002;22: 260-6.).6.Shin JH., Jung HJ., Lee HR., Kim JH., Kim HR., Lee JN. Prevalence, identification, and antimicrobial susceptibility of Staphylococcus lugdunensis from various clinical specimens in Korea. Jpn J Infect Dis. 2007. 60:312–3.7.Moon HW., Lee MA. Two cases of S. lugdunensis isolated from blood and venous catheter. Korean J Clin Microbiol. 2004. 7:90–3. (문희원및이미애. 혈액과정맥도관에서분리된 Staphylococcus lugdunensis 2예. 대한임상미생물학회지 2004;7: 90-3.).8.Kwon O., Uh Y., Hwang GY., Lee JI., Kim HY., Yoon KJ. A case of septicemia by Staphylococcus lugdunensis. Korean J Clin Microbiol. 2007. 10:70–2. (권오건, 어영, 황규열, 이종인, 김효열, 윤갑준. Staphylococcus lugdunensis에 의한 패혈증 1예. 대한임상미생물학회지 2007;10: 70-2.).9.Vandenesch F., Storrs MJ., Poitevin-Later F., Etienne J., Courvalin P., Fleurette J. Delta-like haemolysin produced by Staphylococcus lugdunensis. FEMS Microbiol Lett. 1991. 62:65–8.10.Vandenesch F., Projan SJ., Kreiswirth B., Etienne J., Novick RP. Agr-related sequences in Staphylococcus lugdunensis. FEMS Microbiol Lett. 1993. 111:115–22.11.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Sixteenth informational supplemnet, M100-S16. Wayne, PA: Clinical and Laboratory Standards Institute;2006.12.Pasternack MS., Swartz MN. Lymphadenitis and lymphangitis. Mandell GL, Bennett JE, editors. Principles and practice of infectious disease. 6th ed.Philadelphia: Elsevier;2005. p. 1204–6.
Article13.Gomez-Rodriguez N., Gonzalez-Mediero G., Ibanez-Ruan J., Formigo E. Cellulitis and lymphangitis caused by Staphylococcus lugdunensis. Enferm Infecc Microbiol Clin. 1996. 14:457.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Psoas Abscess Caused by Staphylococcus lugdunensis
- A Case of Botryomycosis Caused by Staphylococcus lugdunensis in a Chronic Alcoholic
- A Case of Septicemia by Staphylococcus lugdunensis
- A Case of Pulmonary Artery Endarteritis due to Staphylococcus lugdunensis in Patient with Clinically Silent Patent Ductus Arteriosus
- A Case of Onychia and Paronychia by Staphylococcus lugdunensis