Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):177-186. 10.14701/ahbps.24-202.
Outcome after spleen-preserving distal pancreatectomy by Warshaw technique for pancreatic body cancer
- Affiliations
-
- 1Pancreas Center, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 2Pancreas Institute, Nanjing Medical University, Nanjing, China
- 3Department of General Surgery, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- 4Department of Radiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
- KMID: 2568266
- DOI: http://doi.org/10.14701/ahbps.24-202
Abstract
- Backgrounds/Aims
Distal pancreatectomy with splenectomy (DPS) is a common surgical procedure for pancreatic body cancer. However, spleen-preserving distal pancreatectomy (SPDP) utilizing the Warshaw technique (WT) in malignancies is generally not favored due to concerns about inadequate resection. This study aims to assess the feasibility and oncologic outcomes of employing SPDP with WT in pancreatic body cancer.
Methods
We conducted a retrospective analysis comparing 21 SPDP patients with 63 DPS patients matched by propensity score from January 2018 to November 2022. Clinical outcomes and follow-up data were analyzed using R.
Results
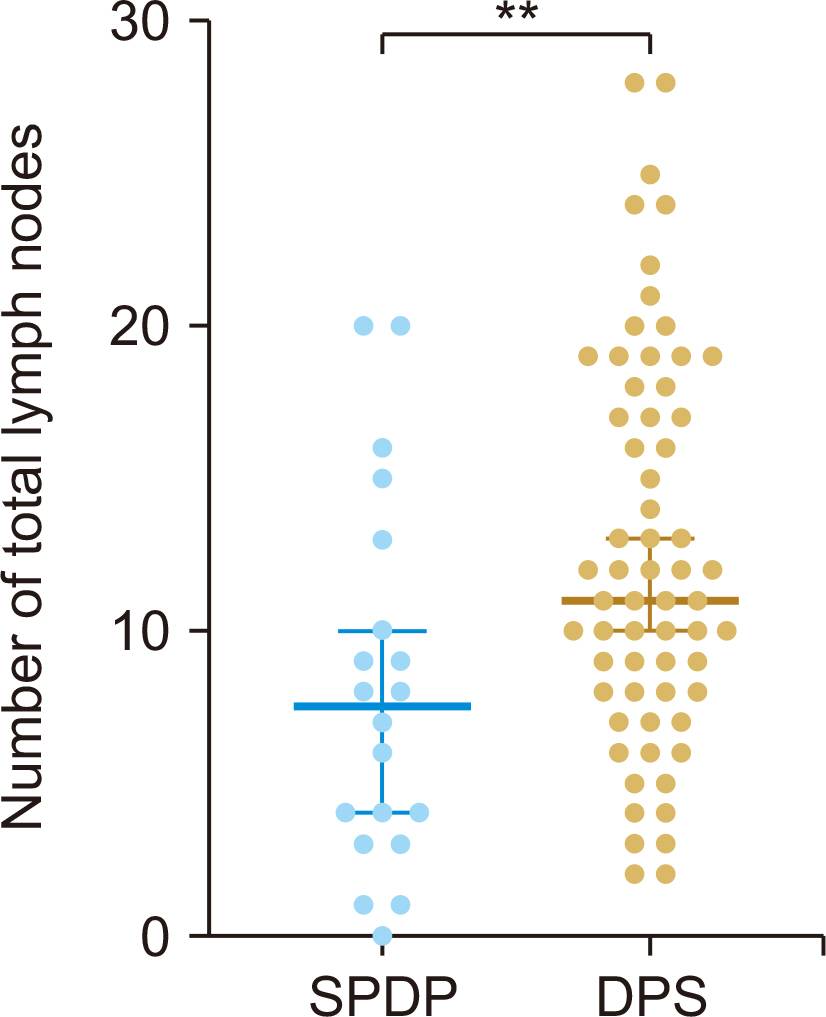
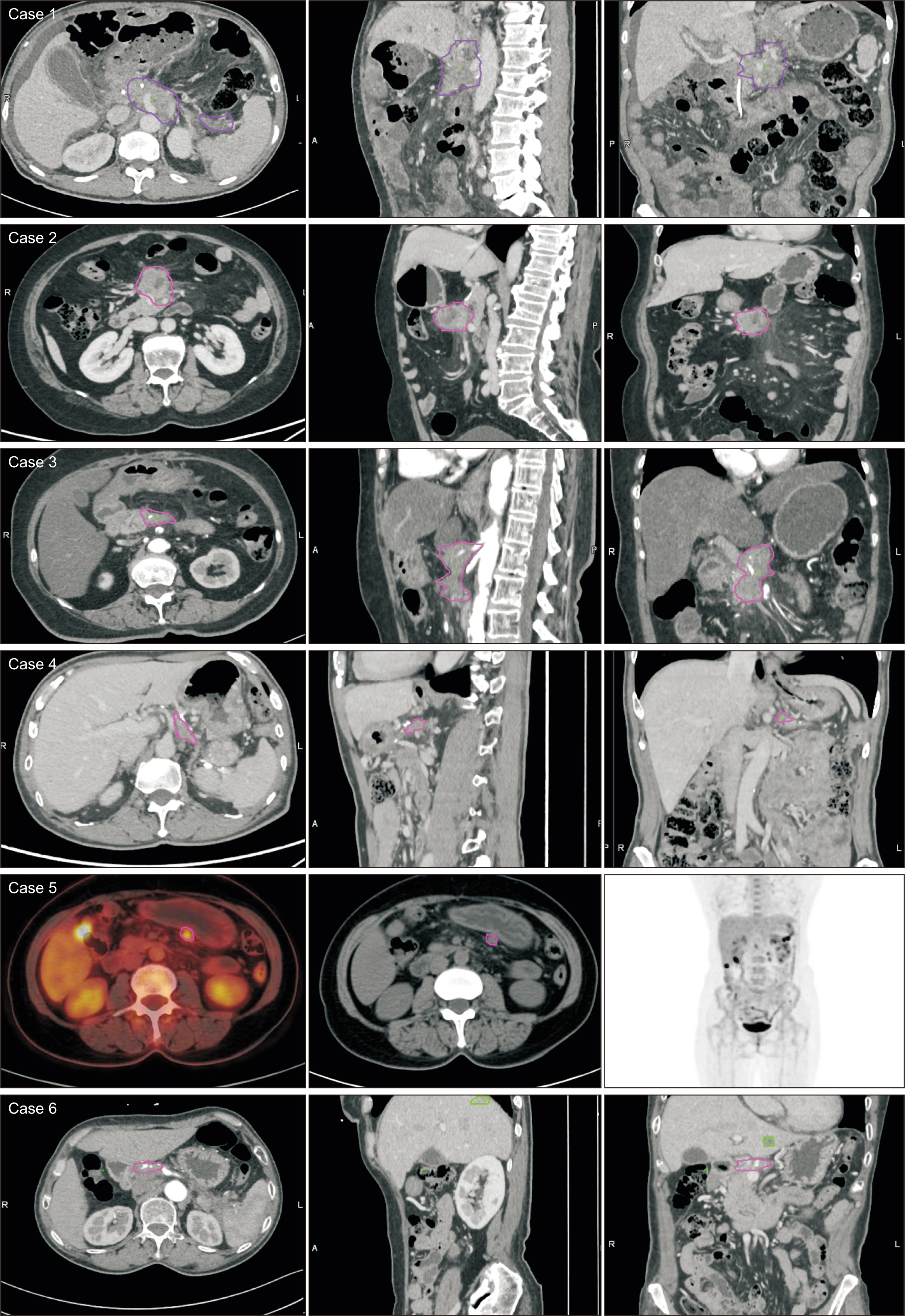
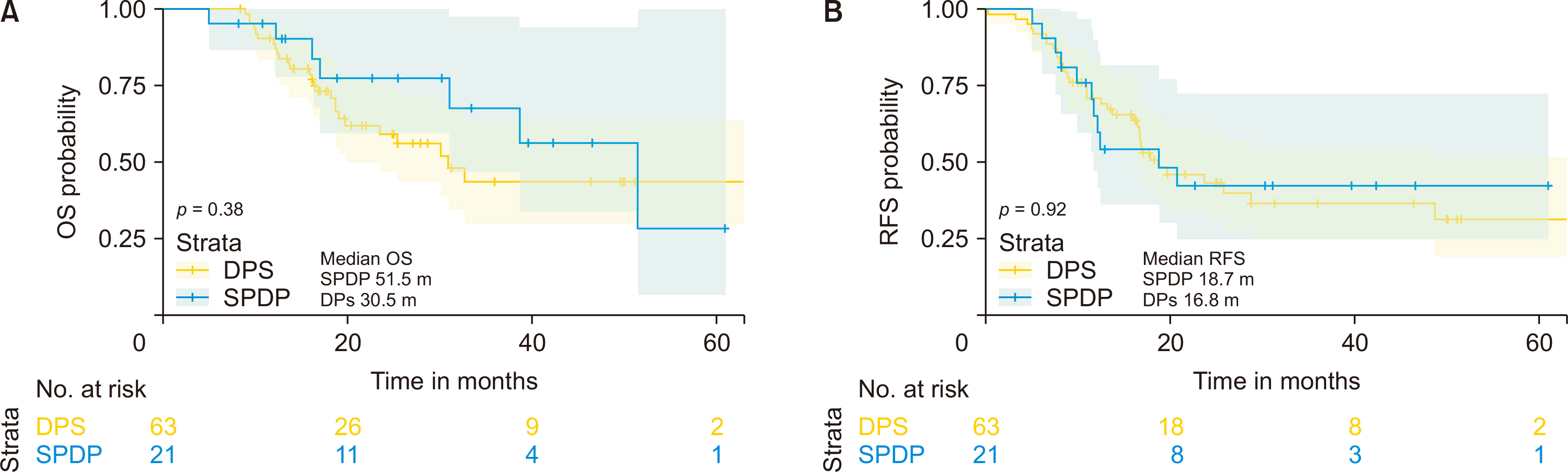
Both groups exhibited similar demographic, intraoperative, and pathological characteristics, with the exception of a reduced number of total lymph nodes (p = 0.006) in the SPDP group. There were no significant differences in the rates of postoperative complications, recurrence, or metastasis. Local recurrence predominantly occurred in the central region as opposed to the spleen region. There were no cases of isolated recurrences in the splenic region. Median overall survival and recurrence-free survival times were 51.5 months for SPDP vs 30.5 months for DPS and 18.7 months vs 16.8 months, respectively (p > 0.05). The incidence of partial splenic infarction and left-side portal hypertension in the SPDP group was 28.6% (6/21) and 9.5% (2/21), respectively, without necessitating splenic abscess puncture, splenectomy, or causing bleeding from perigastric varices.
Conclusions
SPDP did not negatively impact local recurrence or survival rates in selected pancreatic body cancer patients. Further studies are necessary for validation.
Figure
Reference
-
References
1. Siegel RL, Giaquinto AN, Jemal A. 2024; Cancer statistics, 2024. CA Cancer J Clin. 74:12–49. DOI: 10.3322/caac.21820. PMID: 38230766.
Article2. Conroy T, Castan F, Lopez A, Turpin A, Ben Abdelghani M, Wei AC, et al. 2022; Five-year outcomes of FOLFIRINOX vs gemcitabine as adjuvant therapy for pancreatic cancer: a randomized clinical trial. JAMA Oncol. 8:1571–1578. DOI: 10.1001/jamaoncol.2022.3829. PMID: 36048453. PMCID: PMC9437831.3. Fernández-Cruz L, Orduña D, Cesar-Borges G, López-Boado MA. 2005; Distal pancreatectomy: en-bloc splenectomy vs spleen-preserving pancreatectomy. HPB (Oxford). 7:93–98. DOI: 10.1080/13651820510028972. PMID: 18333170. PMCID: PMC2023931.
Article4. Dembinski J, Cannella R, Sauvanet A, Dokmak S. 2022; Laparoscopic spleen-preserving distal pancreatectomy with splenic vessels resection (laparoscopic Warshaw procedure). J Visc Surg. 159:415–423. DOI: 10.1016/j.jviscsurg.2022.03.002. PMID: 35491391.
Article5. Collard M, Marchese T, Guedj N, Cauchy F, Chassaing C, Ronot M, et al. 2019; Is routine splenectomy justified for all left-sided pancreatic cancers? Histological reappraisal of splenic hilar lymphadenectomy. Ann Surg Oncol. 26:1071–1078. DOI: 10.1245/s10434-018-07123-8. PMID: 30607766.
Article6. Kim SH, Kang CM, Satoi S, Sho M, Nakamura Y, Lee WJ. 2013; Proposal for splenectomy-omitting radical distal pancreatectomy in well-selected left-sided pancreatic cancer: multicenter survey study. J Hepatobiliary Pancreat Sci. 20:375–381. DOI: 10.1007/s00534-012-0549-z. PMID: 22911134.
Article7. Warshaw AL. 1988; Conservation of the spleen with distal pancreatectomy. Arch Surg. 123:550–553. DOI: 10.1001/archsurg.1988.01400290032004. PMID: 3358679.
Article8. Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T. 1996; Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 120:885–890. DOI: 10.1016/S0039-6060(96)80099-7. PMID: 8909526.
Article9. Ferrone CR, Konstantinidis IT, Sahani DV, Wargo JA, Fernandez-del Castillo C, Warshaw AL. 2011; Twenty-three years of the Warshaw operation for distal pancreatectomy with preservation of the spleen. Ann Surg. 253:1136–1139. DOI: 10.1097/SLA.0b013e318212c1e2. PMID: 21394008.
Article10. Fujita T, Nakagohri T, Gotohda N, Takahashi S, Konishi M, Kojima M, et al. 2010; Evaluation of the prognostic factors and significance of lymph node status in invasive ductal carcinoma of the body or tail of the pancreas. Pancreas. 39:e48–e54. DOI: 10.1097/MPA.0b013e3181bd5cfa. PMID: 19910836.
Article11. Sahin TT, Fujii T, Kanda M, Nagai S, Kodera Y, Kanzaki A, et al. 2011; Prognostic implications of lymph node metastases in carcinoma of the body and tail of the pancreas. Pancreas. 40:1029–1033. DOI: 10.1097/MPA.0b013e3182207893. PMID: 21705947.
Article12. Malleo G, Maggino L, Nobile S, Casciani F, Cacciatori N, Paiella S, et al. 2020; Reappraisal of nodal staging and study of lymph node station involvement in distal pancreatectomy for body-tail pancreatic ductal adenocarcinoma. Eur J Surg Oncol. 46:1734–1741. DOI: 10.1016/j.ejso.2020.04.006. PMID: 32327367.
Article13. Tanaka K, Kimura Y, Hayashi T, Ambo Y, Yoshida M, Umemoto K, et al. 2022; Appropriate lymph node dissection sites for cancer in the body and tail of the pancreas: a multicenter retrospective study. Cancers (Basel). 14:4409. DOI: 10.3390/cancers14184409. PMID: 36139569. PMCID: PMC9497245.
Article14. Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. 2020; The 2019 WHO classification of tumours of the digestive system. Histopathology. 76:182–188. DOI: 10.1111/his.13975. PMID: 31433515. PMCID: PMC7003895.
Article15. Allen PJ, Kuk D, Castillo CF, Basturk O, Wolfgang CL, Cameron JL, et al. 2017; Multi-institutional validation study of the American Joint Commission on Cancer (8th Edition) changes for T and N staging in patients with pancreatic adenocarcinoma. Ann Surg. 265:185–191. DOI: 10.1097/SLA.0000000000001763. PMID: 27163957. PMCID: PMC5611666.
Article16. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. International Study Group on Pancreatic Surgery (ISGPS). 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.
Article17. Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. 2007; Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 142:20–25. DOI: 10.1016/j.surg.2007.02.001. PMID: 17629996.
Article18. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. 2007; Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 142:761–768. DOI: 10.1016/j.surg.2007.05.005. PMID: 17981197.
Article19. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.20. Cesta MF. 2006; Normal structure, function, and histology of the spleen. Toxicol Pathol. 34:455–465. DOI: 10.1080/01926230600867743. PMID: 17067939.
Article21. Tsiouris A, Cogan CM, Velanovich V. 2011; Distal pancreatectomy with or without splenectomy: comparison of postoperative outcomes and surrogates of splenic function. HPB (Oxford). 13:738–744. DOI: 10.1111/j.1477-2574.2011.00369.x. PMID: 21929675. PMCID: PMC3210976.
Article22. He Z, Qian D, Hua J, Gong J, Lin S, Song Z. 2014; Clinical comparison of distal pancreatectomy with or without splenectomy: a meta-analysis. PLoS One. 9:e91593. DOI: 10.1371/journal.pone.0091593. PMID: 24682038. PMCID: PMC3969315.
Article23. Pendola F, Gadde R, Ripat C, Sharma R, Picado O, Lobo L, et al. 2017; Distal pancreatectomy for benign and low grade malignant tumors: short-term postoperative outcomes of spleen preservation-A systematic review and update meta-analysis. J Surg Oncol. 115:137–143. DOI: 10.1002/jso.24507. PMID: 28133818.
Article24. Shi N, Liu SL, Li YT, You L, Dai MH, Zhao YP. 2016; Splenic preservation versus splenectomy during distal pancreatectomy: a systematic review and meta-analysis. Ann Surg Oncol. 23:365–374. DOI: 10.1245/s10434-015-4870-z. PMID: 26493758.
Article25. Buzelé R, Barbier L, Sauvanet A, Fantin B. 2016; Medical complications following splenectomy. J Visc Surg. 153:277–286. DOI: 10.1016/j.jviscsurg.2016.04.013. PMID: 27289254.
Article26. Sun LM, Chen HJ, Jeng LB, Li TC, Wu SC, Kao CH. 2015; Splenectomy and increased subsequent cancer risk: a nationwide population-based cohort study. Am J Surg. 210:243–251. DOI: 10.1016/j.amjsurg.2015.01.017. PMID: 25986002.
Article27. Giger U, Michel JM, Wiesli P, Schmid C, Krähenbühl L. 2006; Laparoscopic surgery for benign lesions of the pancreas. J Laparoendosc Adv Surg Tech A. 16:452–457. DOI: 10.1089/lap.2006.16.452. PMID: 17004867.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spleen-Preserving Distal Pancreatectomy for Blunt Pancreatic Trauma in a Pediatric Patient
- Clinical course of pancreas cancer diagnosed after spleen-preserving distal pancreatectomy with borderline lesion: two case reports
- Robotic single-port plus one-port splenic vessel-conserving spleen-preserving distal pancreatectomy: a case report
- "Extended" Distal Pancreatectomy with Segmental Resection of Both Splenic Vessels; Extended Warshaw's Procedure
- Dual-incision laparoscopic spleen-preserving distal pancreatectomy