J Korean Neurosurg Soc.
2025 May;68(3):360-368. 10.3340/jkns.2024.0176.
Efficacy of Anti-Adhesive Substitute and Step-by-Step Techniques in Decompressive Craniectomy and Subsequent Cranioplasty
- Affiliations
-
- 1Department of Neurosurgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2567467
- DOI: http://doi.org/10.3340/jkns.2024.0176
Abstract
Objective
: Dural substitutes have been widely used in decompressive craniectomy to prevent adhesion, and have significantly reduced blood loss and operation time. However, there are only limited studies providing information regarding detailed techniques and the specific operation time that is associated with good prognoses. In this study, we evaluate the effectiveness of using a dural substitute as an anti-adhesive material during cranioplasty, focusing on technical details and operation time from incision to bone closure.
Methods
: A retrospectively reviewed total of 66 patients were included who underwent a craniectomy and subsequent cranioplasty caused by either a severe traumatic brain injury (n=35) or malignant infarction (n=31). The patients were divided into two groups depending on whether Neuro-Patch was used or not (31 in the Neuro-Patch group, 35 in the non-Neuro-Patch group). Propensity score matching was used to minimize the differences. Associated morbidities as well as operation time, and blood loss were analyzed and compared between the two groups.
Results
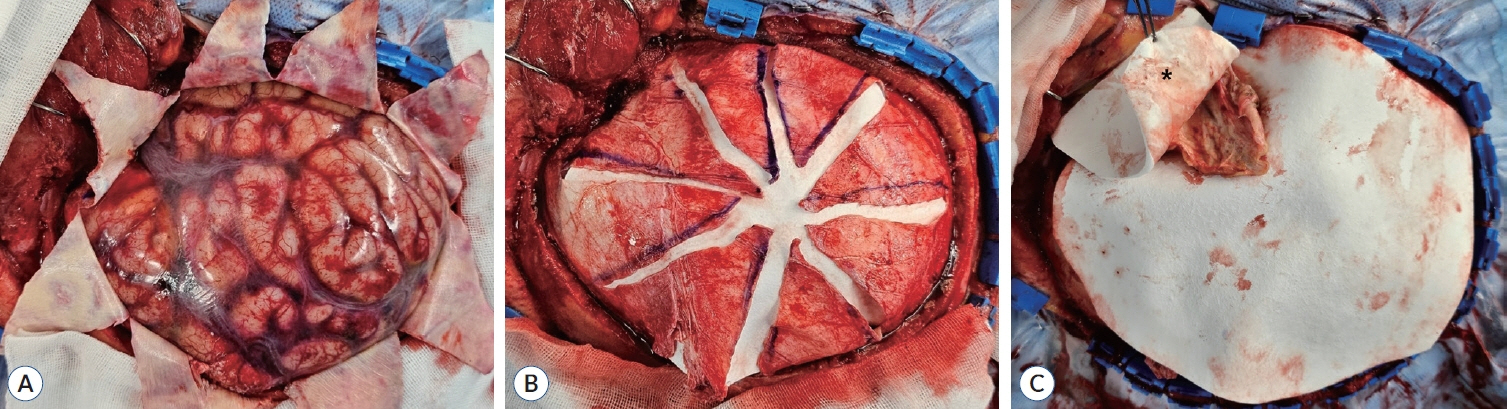
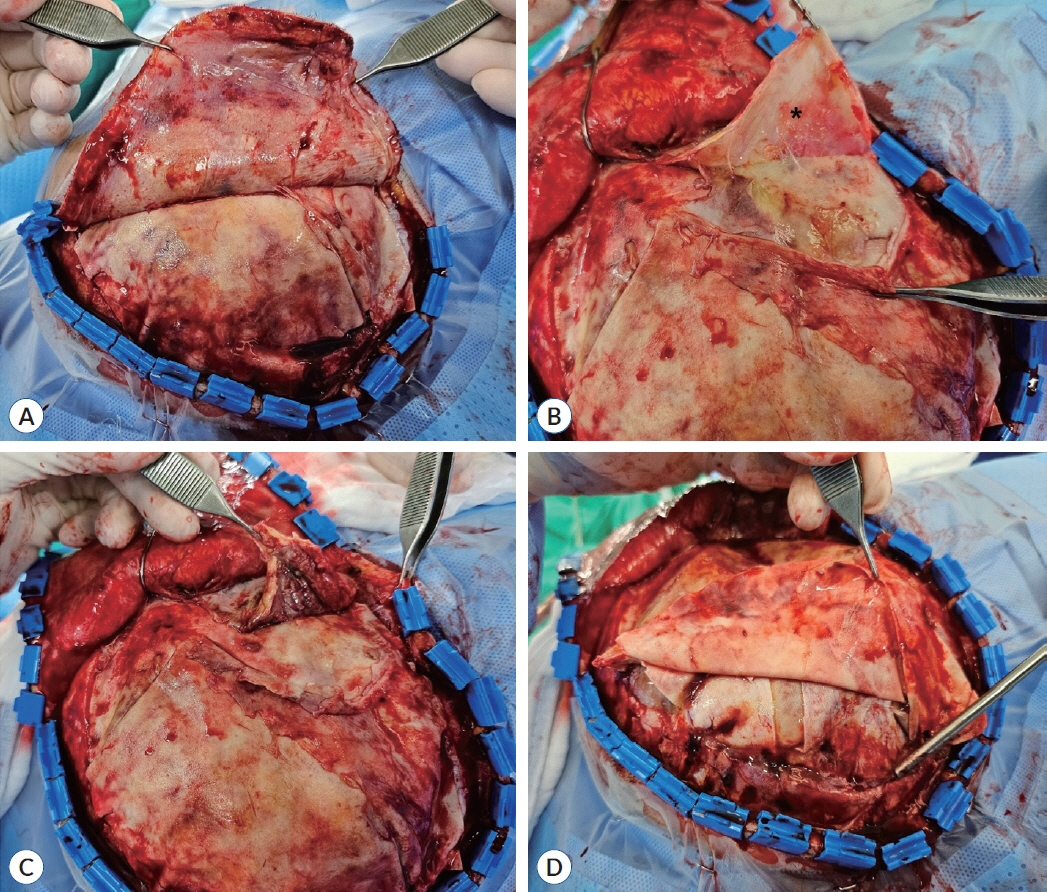
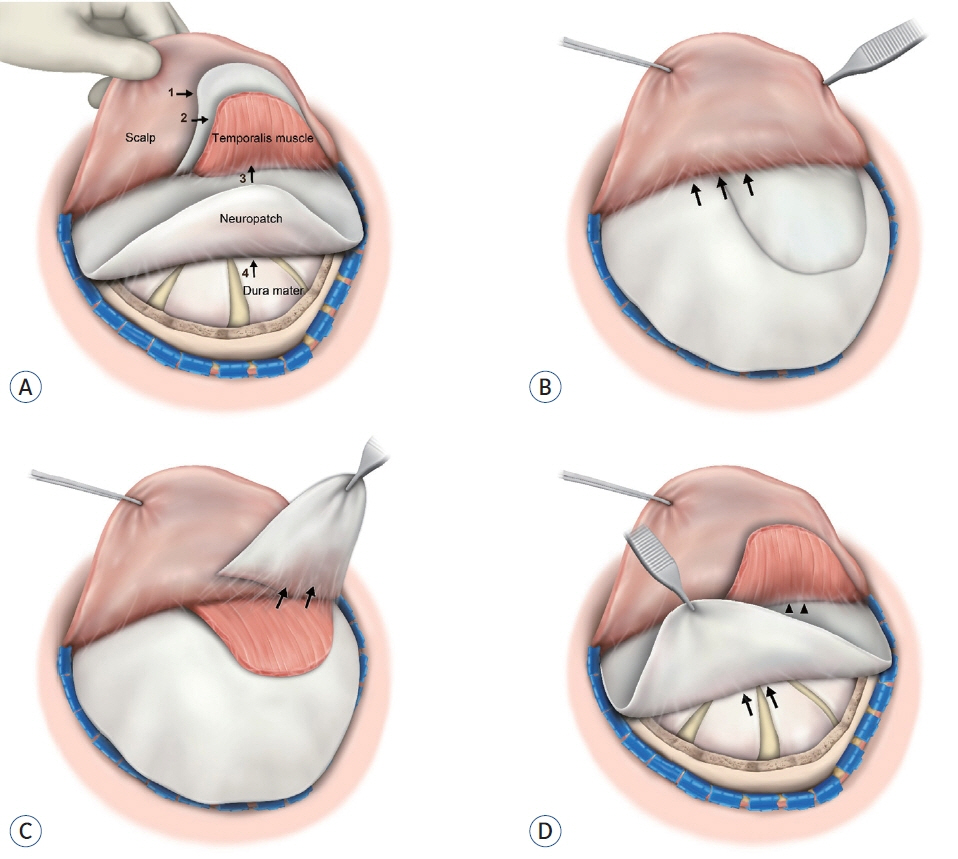
: To prevent adhesion, Neuro-Patch was placed as an onlay, enough to cover the surrounding skull at least 1 cm beyond the bone edges. A small piece was also placed over the temporalis muscle during the craniectomy. A step-by-step dissection was performed to minimize retraction-related injury during the subsequent cranioplasty. The mean estimated blood loss was significantly lower in the Neuro-Patch group (54.6±34.9 vs. 149.0±70.8 mL, p<0.001) and the mean time from incision to bone closure in the Neuro-Patch group was 40.8±14.3 minutes, which was significantly lower than in the non-Neuro-Patch group (91.5±38.2 minutes) as well. For each analysis of complications, the differences were not significant, however, the overall complication rate was significantly lower in the Neuro-Patch group (9.7%) than in the non-Neuro-Patch group (42.9%).
Conclusion
: Neuro-Patch can be used safely and effectively as an anti-adhesive substitute during cranioplasty. To improve clinical outcomes as well as intraoperative parameters including the time from incision to bone closure, planned placement of Neuro-Patch during craniectomy and the step-by-step dissection during cranioplasty is important.
Keyword
Figure
Reference
-
References
1. Colgan NC, Cronin MM, Gobbo OL, O'Mara SM, O'Connor WT, Gilchrist MD. Quantitative MRI analysis of brain volume changes due to controlled cortical impact. J Neurotrauma. 27:1265–1274. 2010.
Article2. Geurts M, van der Worp HB, Kappelle LJ, Amelink GJ, Algra A, Hofmeijer J, et al. Surgical decompression for space-occupying cerebral infarction: outcomes at 3 years in the randomized HAMLET trial. Stroke. 44:2506–2508. 2013.
Article3. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 26:E9. 2009.
Article4. Huang YH, Lee TC, Chen WF, Wang YM. Safety of the nonabsorbable dural substitute in decompressive craniectomy for severe traumatic brain injury. J Trauma. 71:533–537. 2011.
Article5. Jeong TS, Kim WK, Jang MJ. Cranioplasty results after the use of a polyester urethane dural substitute (Neuro-Patch®) as an adhesion prevention material in traumatic decompressive craniectomy. J Trauma Inj. 32:195–201. 2019.
Article6. Khalili H, Omidvar A, Ghaffarpasand F, Yadollahikhales G. Cranioplasty results after application of anti-adhesive films (OrthoWrap™) in traumatic decompressive craniectomy. Bull Emerg Trauma. 4:24–28. 2016.7. Kim H, Sung SO, Kim SJ, Kim SR, Park IS, Jo KW. Analysis of the factors affecting graft infection after cranioplasty. Acta Neurochir (Wien). 155:2171–2176. 2013.
Article8. Kim SP, Kang DS, Cheong JH, Kim JH, Song KY, Kong MH. Clinical analysis of epidural fluid collection as a complication after cranioplasty. J Korean Neuro surg Soc. 56:410–418. 2014.
Article9. Missori P, Polli FM, Peschillo S, D'Avella E, Paolini S, Miscusi M. Double dural patch in decompressive craniectomy to preserve the temporal muscle: technical note. Surg Neurol. 70:437–439. discussion 439. 2008.
Article10. Oladunjoye AO, Schrot RJ, Zwienenberg-Lee M, Muizelaar JP, Shahlaie K. Decompressive craniectomy using gelatin film and future bone flap replacement. J Neurosurg. 118:776–782. 2013.
Article11. Pathrose Kamalabai R, Nagar M, Chandran R, Mohammed Haneefa Suharanbeevi S, Bhanu Prabhakar R, Peethambaran A, et al. Rationale behind the use of double-layer polypropylene patch (G-patch) dural substitute during decompressive craniectomy as an adhesion preventive material for subsequent cranioplasty with special reference to flap elevation time. World Neurosurg. 111:e105–e112. 2018.
Article12. Pierson M, Birinyi PV, Bhimireddy S, Coppens JR. Analysis of decompressive craniectomies with subsequent cranioplasties in the presence of collagen matrix dural substitute and polytetrafluoroethylene as an adhesion preventative material. World Neurosurg. 86:153–160. 2016.
Article13. Quinn TM, Taylor JJ, Magarik JA, Vought E, Kindy MS, Ellegala DB. Decompressive craniectomy: technical note. Acta Neurol Scand. 123:239–244. 2011.
Article14. Raghavan A, Wright JM, Huang Wright C, Sajatovic M, Miller J. Effect of dural substitute and technique on cranioplasty operative metrics: a systematic literature review. World Neurosurg. 119:282–289. 2018.
Article15. Sun H, Wang H, Diao Y, Tu Y, Li X, Zhao W, et al. Large retrospective study of artificial dura substitute in patients with traumatic brain injury undergo decompressive craniectomy. Brain Behav. 8:e00907. 2018.
Article16. Vakis A, Koutentakis D, Karabetsos D, Kalostos G. Use of polytetrafluoroethylene dural substitute as adhesion preventive material during craniectomies. Clin Neurol Neurosurg. 108:798–802. 2006.
Article17. von Wild KR. Examination of the safety and efficacy of an absorbable dura mater substitute (Dura Patch) in normal applications in neurosurgery. Surg Neurol. 52:418–424. discussion 425. 1999.
Article18. Walcott BP, Kwon CS, Sheth SA, Fehnel CR, Koffie RM, Asaad WF, et al. Predictors of cranioplasty complications in stroke and trauma patients. J Neurosurg. 118:757–762. 2013.
Article19. Wright JM, Raghavan A, Wright CH, Alonso A, Momotaz H, Sweet J, et al. Impact of dual-layer duraplasty during hemicraniectomy on morbidity and operative metrics of cranioplasty: a retrospective case-control study comparing a single-layer with a dual-layer technique. World Neurosurg. 125:e1189–e1195. 2019.
Article20. Zhang Q, Li Y, Chang X. Role of decompressive craniectomy in the management of traumatic brain injury - a meta-analysis of randomized controlled trials. Ann Indian Acad Neurol. 26:966–974. 2023.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Review of Cranioplasty after Decompressive Craniectomy
- Paradoxical Herniation after Decompressive Craniectomy for Acute Subdural Hematoma
- Cranioplasty Results after the Use of a Polyester Urethane Dural Substitute (Neuro-Patch®) as an Adhesion Prevention Material in Traumatic Decompressive Craniectomy
- Hydrocephalus Developed after Cranioplasty: Influence of Cranioplasty on the CSF Circulation
- Safety and Efficacy of Early Cranioplasty after Decompressive Craniectomy in Traumatic Brain Injury Patients