Cancer Res Treat.
2025 Apr;57(2):539-546. 10.4143/crt.2024.879.
Determinants of Prostate Cancer Screening in Korean Men: A Nationwide Study Using the Korean National Cancer Screening Survey 2023
- Affiliations
-
- 1Department of Cancer Control and Population Health, National Cancer Center Graduate School of Cancer Science and Policy, Goyang, Korea
- 2National Cancer Control Institute, National Cancer Center, Goyang, Korea
- KMID: 2566870
- DOI: http://doi.org/10.4143/crt.2024.879
Abstract
- Purpose
Research on the prevalence of prostate cancer (PCa) screening and reasons for undergoing screening is limited. We aimed to identify the factors influencing PCa screening behavior and explore the underlying motivations among Korean men.
Materials and Methods
This cross-sectional study used data from the 2023 Korean National Cancer Screening Survey, which employs a nationally representative random sampling method. This study included 1,784 men aged 40-74 years. The respondents reported their experiences with PCa screening. Multivariable logistic regression analysis was conducted to identify the factors associated with participation in PCa screening.
Results
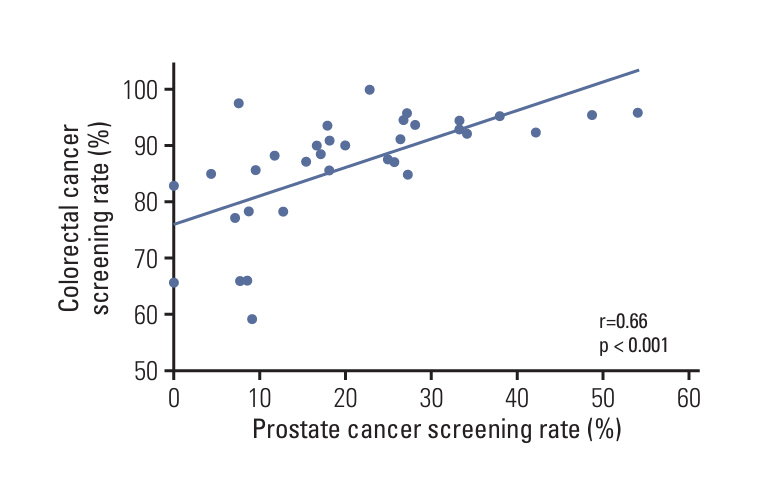
The lifetime PCa screening rate was 18.6%. Among screening modalities, transrectal ultrasonography was the most frequently used (31.9%), followed by prostate-specific antigen tests (25.6%) and digital rectal examinations (21.5%). The multivariable analysis identified several factors that significantly increased the likelihood of screening participation, including older age, living with a spouse, poor self-reported health, and abstinence from alcohol consumption in the previous 12 months. Men who had undergone colorectal cancer screening were more likely to participate in PCa screening (adjusted odds ratio, 4.01; 95% confidence interval, 2.03 to 7.93) than those who had not. The primary motivations for screening were recommendations from family or social networks (31.9%) and inclusion in health examination packages (24.3%), whereas healthcare provider recommendations (18%) and symptomatic concerns (5.7%) were the least influential.
Conclusion
Our findings highlight the importance of providing evidence-based information for PCa screening recommendations and the need for improved communication and implementation of a shared decision-making approach for PCa screening in Korea.
Figure
Reference
-
References
1. Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024; 74:229–63.
Article2. Han SH, Yuk HD. Epidemiology of urologic cancer in Korea: nationwide trends in the last 2 decades. J Urol Oncol. 2023; 21:32–44.
Article3. Pak S, Jung KW, Park EH, Ko YH, Won YJ, Joung JY. Incidence and mortality projections for major cancers among Korean men until 2034, with a focus on prostate cancer. Investig Clin Urol. 2022; 63:175–83.
Article4. Boyle P, Severi G, Giles GG. The epidemiology of prostate cancer. Urol Clin North Am. 2003; 30:209–17.
Article5. Bostwick DG, Burke HB, Djakiew D, Euling S, Ho SM, Landolph J, et al. Human prostate cancer risk factors. Cancer. 2004; 101:2371–490.
Article6. Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019; 10:63–89.
Article7. U. S. Preventive Services Task Force, Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018; 319:1901–13.8. Wei JT, Barocas D, Carlsson S, Coakley F, Eggener S, Etzioni R, et al. Early Detection of prostate cancer: AUA/SUO guideline part I: prostate cancer screening. J Urol. 2023; 210:46–53.
Article9. Cui T, Kovell RC, Terlecki RP. Is it time to abandon the digital rectal examination? Lessons from the PLCO Cancer Screening Trial and peer-reviewed literature. Curr Med Res Opin. 2016; 32:1663–9.
Article10. Ilic D, Djulbegovic M, Jung JH, Hwang EC, Zhou Q, Cleves A, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ. 2018; 362:k3519.
Article11. Martin RM, Donovan JL, Turner EL, Metcalfe C, Young GJ, Walsh EI, et al. Effect of a low-intensity PSA-based screening intervention on prostate cancer mortality: the CAP randomized clinical trial. JAMA. 2018; 319:883–95.
Article12. Naji L, Randhawa H, Sohani Z, Dennis B, Lautenbach D, Kavanagh O, et al. Digital rectal examination for prostate cancer screening in primary care: a systematic review and meta-analysis. Ann Fam Med. 2018; 16:149–54.
Article13. Nam R, Patel C, Milot L, Hird A, Wallis C, Macinnis P, et al. Prostate MRI versus PSA screening for prostate cancer detection (the MVP Study): a randomised clinical trial. BMJ Open. 2022; 12:e059482.
Article14. Wurnschimmel C, Chandrasekar T, Hahn L, Esen T, Shariat SF, Tilki D. MRI as a screening tool for prostate cancer: current evidence and future challenges. World J Urol. 2023; 41:921–8.
Article15. Lee EN, Park JH, Kang SG, Yun S, Sin KM, Kim KM. Factors affecting prostate cancer screening behavior. Asian Oncol Nurs. 2015; 15:256–63.
Article16. Lee E, Park Y, Park J. Knowledge, health beliefs and screening status of prostate cancer among middle-aged and elderly men. Open J Nurs. 2016; 6:672–87.
Article17. Suh M, Choi KS, Lee YY, Jun JK. Trends in cancer screening rates among Korean men and women: results from the Korean National Cancer Screening Survey, 2004-2012. Cancer Res Treat. 2013; 45:86–94.
Article18. Hong S, Lee YY, Lee J, Kim Y, Choi KS, Jun JK, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004-2018. Cancer Res Treat. 2021; 53:330–8.
Article19. Lee K, Lee YY, Suh M, Jun JK, Park B, Kim Y, et al. Impact of COVID-19 on cancer screening in South Korea. Sci Rep. 2022; 12:11380.
Article20. Pyun JH, Kang SH, Kim JY, Shin JE, Jeong IG, Kim JW, et al. Survey results on the perception of prostate-specific antigen and prostate cancer screening among the general public. Korean J Urol Oncol. 2020; 18:40–6.
Article21. Ko YH, Roh KC, Kim BH. The national-wide incidence of prostate-specific antigen testing trend for a decade in Korea by age group. Investig Clin Urol. 2022; 63:184–91.
Article22. Guessous I, Cullati S, Fedewa SA, Burton-Jeangros C, Courvoisier DS, Manor O, et al. Prostate cancer screening in Switzerland: 20-year trends and socioeconomic disparities. Prev Med. 2016; 82:83–91.
Article23. Ilunga Tshiswaka D, Donley T, Okafor A, Memiah P, Mbizo J. Prostate and colorectal cancer screening uptake among US and foreign-born males: evidence from the 2015 NHIS survey. J Community Health. 2017; 42:612–23.
Article24. Morere JF, Touboul C, Lhomel C, Roupret M. Prostate cancer screening in France: results from the EDIFICE surveys. Prog Urol. 2020; 30:332–8.25. Drazer MW, Huo D, Schonberg MA, Razmaria A, Eggener SE. Population-based patterns and predictors of prostate-specific antigen screening among older men in the United States. J Clin Oncol. 2011; 29:1736–43.
Article26. Li J, Zhao G, Hall IJ. Pre-screening discussions and prostate-specific antigen testing for prostate cancer screening. Am J Prev Med. 2015; 49:259–63.
Article27. Tchir D, Farag M, Szafron M. Prostate-specific antigen (PSA) screening rates and factors associated with screening in Eastern Canadian men: findings from cross-sectional survey data. Can Urol Assoc J. 2020; 14:E319–27.28. Jung W, Cho IY, Jeon KH, Yeo Y, Jun JK, Suh M, et al. A web-based decision aid for informed prostate cancer screening: development and pilot evaluation. J Korean Med Sci. 2023; 38:e360.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in Cancer-Screening Rates in Korea: Findings from the National Cancer Screening Survey, 2004-2023
- A Cost-Benefit Comparison of Biparametric Magnetic Resonance Imaging Versus Conventional Prostate Cancer Screening
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2011
- Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004–2018
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2010