J Korean Neurosurg Soc.
2025 Mar;68(2):150-158. 10.3340/jkns.2024.0172.
Posterior Lumbar Element Enforcement by Decompression Alone with Interspinous Fixation without Interbody Fusion for the Surgical Management of Lumbar Spondylolisthesis
- Affiliations
-
- 1Department of Neurosurgery, Gwangju Heemang Hospital, Gwangju, Korea
- 2Department of Neurosurgery, Chonnam National University Medical School & Research Institute of Medical Sciences, Gwangju, Korea
- 3Division of Rheumatology, Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2565273
- DOI: http://doi.org/10.3340/jkns.2024.0172
Abstract
Objective
: In degenerative lumbar spondylolisthesis, interbody fusion surgery (IFS) has long been recommended as the gold standard of surgical management. However, IFS is less recommended for high-risk patients such as the elderly because it involves extensive surgery, with a long operation time and high volumes of blood loss, which lead to marked perioperative morbidity. We report an alternative primary and salvage treatment technique for high-risk lumbar spondylolisthesis through posterior lumbar element reinforcement using interspinous fixation and decompression alone without interbody fusion.
Methods
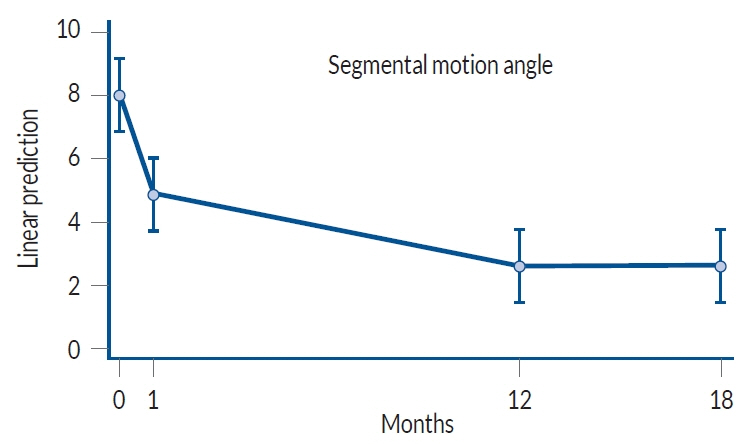
: Plain radiographs, computed tomography scans, and magnetic resonance imaging, taken at different intervals, were used to measure local disc height (DH), vertebral body slippage (BS), and segmental motion angle (SMA). A Visual analogue scale and the Oswestry disability index (ODI) were applied pre-operation and at the last follow-up.
Results
: The local SMA decreased significantly by 3.46°±3.07°, from 10.61°±3.42° preoperatively to 7.15±3.70 at the last follow-up (p<0.001). The DH decreased from 8.61±2.88 mm preoperatively to 8.41±2.48 mm at the last follow-up (p=0.074). The BS decreased from 3.49±4.29 mm preoperatively to 3.41±4.91 mm at the last follow-up (p=0.092). None of the patients reported worsening pain or an increased ODI after surgery, and there were no surgery-related complications.
Conclusion
: Posterior lumbar element reinforcement by decompression alone with SPIRE™ fixation is an alternative primary and salvage treatment option for select patients with spondylolisthesis.
Keyword
Figure
Reference
-
References
1. Austevoll IM, Hermansen E, Fagerland MW, Storheim K, Brox JI, Solberg T, et al. Decompression with or without fusion in degenerative lumbar spondylolisthesis. N Engl J Med. 385:526–538. 2021.
Article2. Chan AK, Sharma V, Robinson LC, Mummaneni PV. Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg Clin N Am. 30:353–364. 2019.
Article3. DiPaola CP, Molinari RW. Posterior lumbar interbody fusion. J Am Acad Orthop Surg. 16:130–139. 2008.
Article4. Kaibara T, Karahalios DG, Porter RW, Kakarla UK, Reyes PM, Choi SK, et al. Biomechanics of a lumbar interspinous anchor with transforaminal lumbar interbody fixation. World Neurosurg. 73:572–577. 2010.
Article5. Karahalios DG, Kaibara T, Porter RW, Kakarla UK, Reyes PM, Baaj AA, et al. Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. J Neurosurg Spine. 12:372–380. 2010.
Article6. Kim HJ, Bak KH, Chun HJ, Oh SJ, Kang TH, Yang MS. Posterior interspinous fusion device for one-level fusion in degenerative lumbar spine disease : comparison with pedicle screw fixation - preliminary report of at least one year follow up. J Korean Neurosurg Soc. 52:359–364. 2012.
Article7. Koslosky E, Gendelberg D. Classification in brief: the Meyerding classification system of spondylolisthesis. Clin Orthop Relat Res. 478:1125–1130. 2020.
Article8. Lin PM. Posterior lumbar interbody fusion technique: complications and pitfalls. Clin Orthop Relat Res. 193:90–102. 1985.9. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 1:2–18. 2015.10. Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 88:2714–2720. 2006.
Article11. Steiger F, Becker HJ, Standaert CJ, Balague F, Vader JP, Porchet F, et al. Surgery in lumbar degenerative spondylolisthesis: indications, outcomes and complications. A systematic review. Eur Spine J. 23:945–973. 2014.
Article12. Stillerman CB, Schneider JH, Gruen JP. Evaluation and management of spondylolysis and spondylolisthesis. Clin Neurosurg. 40:384–415. 1993.13. Wang JC, Haid RW Jr, Miller JS, Robinson JC. Comparison of CD HORIZON SPIRE spinous process plate stabilization and pedicle screw fixation after anterior lumbar interbody fusion: invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2005. J Neurosurg Spine. 4:132–136. 2006.
Article14. Wang JC, Spenciner D, Robinson JC. SPIRE spinous process stabilization plate: biomechanical evaluation of a novel technology: invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2005. J Neurosurg Spine. 4:160–164. 2006.
Article15. Watters WC 3rd, Bono CM, Gilbert TJ, Kreiner DS, Mazanec DJ, Shaffer WO, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 9:609–614. 2009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Lumbar Interbody Fusion and Graf Band Fixation for Lumbar Isthmic Spondylolisthesis
- Intertransverse Fusion in Spondylolisthesis: Report of a Case
- A Comparison of Posterolateral and Posterior Interbody Fusion in the Surgical Treatment of Lumbar Spondylolisthesis
- Comparison between Posterior Lumbar Interbody Fusion with Pedicle Screw Fixation and Posterolateral Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis in Adults
- Posterior Lumbar Interbody Fusion