J Korean Diabetes.
2024 Dec;25(4):217-223. 10.4093/jkd.2024.25.4.217.
Sleep and Diabetes
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
- KMID: 2563239
- DOI: http://doi.org/10.4093/jkd.2024.25.4.217
Abstract
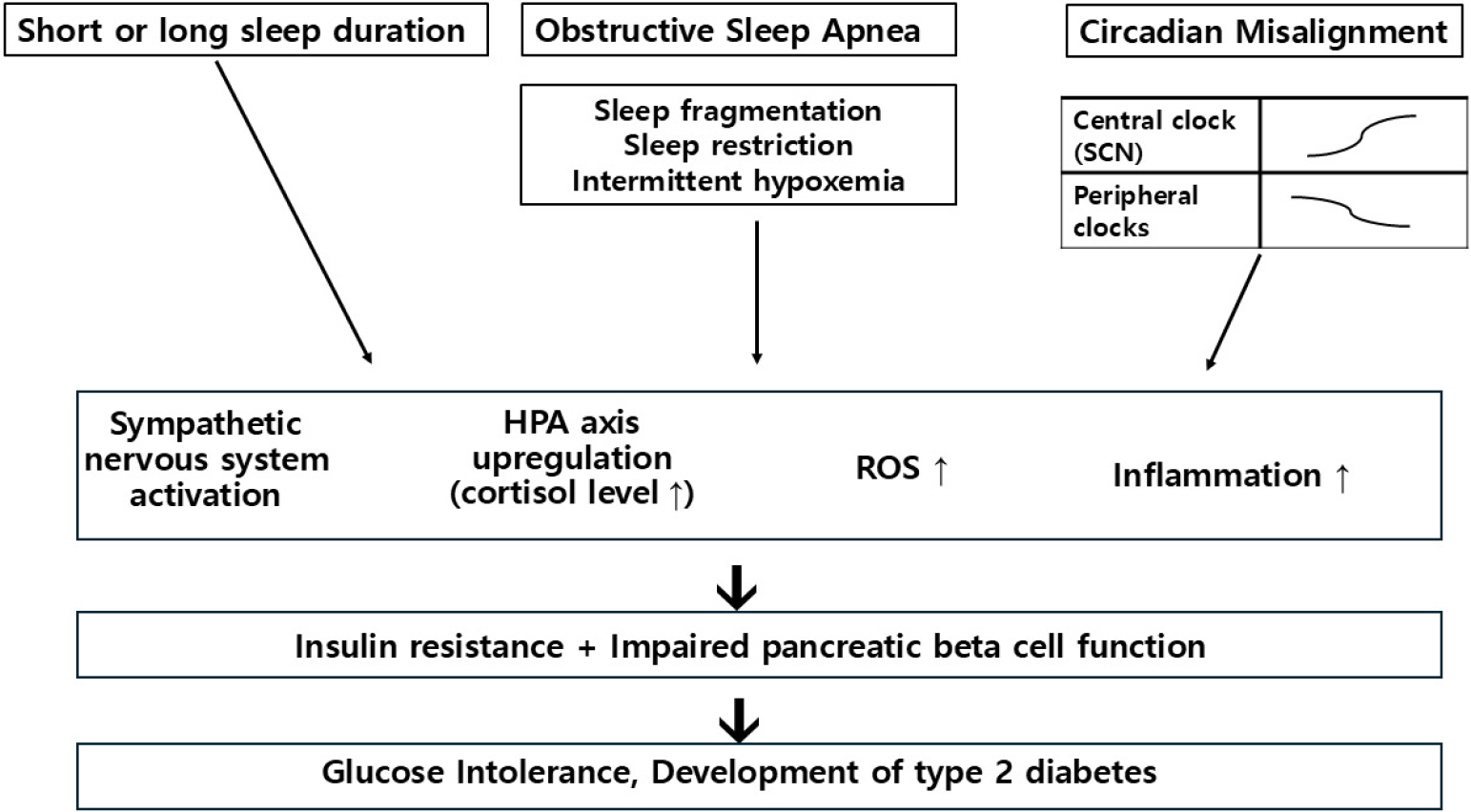
- Modern society has significantly altered sleep patterns compared to those of the past, leading to an increased prevalence of sleep and circadian rhythm disorders. Numerous studies over the past decades have provided substantial evidence that these disorders negatively impact cognitive function, work performance, and the incidence and mortality of cardiovascular diseases. Recent interest in the effects of sleep and circadian rhythm disturbances on glucose metabolism has surged, with growing recognition of sleep’s critical role in regulating glucose homeostasis and appetite. Sleep disturbances contribute to the global rise in obesity and type 2 diabetes, necessitating a thorough understanding of how sleep affects glucose metabolism and whether interventions for sleep disorders can positively impact metabolic outcomes. This review explores the relationship among sleep duration, quality, and glucose metabolism, focusing on the mechanisms underlying these associations. It examines epidemiological and experimental studies demonstrating that insufficient or poor-quality sleep adversely affects glucose regulation. The review highlights the impact of sleep disorders, such as insomnia and obstructive sleep apnea, on glucose metabolism and outlines potential interventions, including cognitive behavioral therapy and pharmacological treatments, that may improve sleep quality and metabolic control.
Keyword
Figure
Reference
-
1.Shan Z., Ma H., Xie M., Yan P., Guo Y., Bao W, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015. 38:529–37.
Article2.Nôga DA., Meth EMES., Pacheco AP., Tan X., Cedernaes J., van Egmond LT, et al. Habitual short sleep duration, diet, and development of type 2 diabetes in adults. JAMA Netw Open. 2024. 7:e241147.
Article3.Briançon-Marjollet A., Weiszenstein M., Henri M., Thomas A., Godin-Ribuot D., Polak J. The impact of sleep disorders on glucose metabolism: endocrine and molecular mechanisms. Diabetol Metab Syndr. 2015. 7:25.
Article4.Koopman ADM., Beulens JW., Dijkstra T., Pouwer F., Bremmer MA., van Straten A, et al. Prevalence of insomnia (symptoms) in T2D and association with metabolic param-eters and glycemic control: meta-analysis. J Clin Endocrinol Metab. 2020. 105:614–43.
Article5.Parameswaran G., Ray DW. Sleep, circadian rhythms, and type 2 diabetes mellitus. Clin Endocrinol (Oxf). 2022. 96:12–20.
Article6.Schipper SBJ., Van Veen MM., Elders PJM., van Straten A., Van Der Werf YD., Knutson KL, et al. Sleep disorders in people with type 2 diabetes and associated health outcomes: a review of the literature. Diabetologia. 2021. 64:2367–77.
Article7.Reutrakul S., Mokhlesi B. Obstructive sleep apnea and diabetes: a state of the art review. Chest. 2017. 152:1070–86.8.West SD., Groves DC., Lipinski HJ., Nicoll DJ., Mason RH., Scanlon PH, et al. The prevalence of retinopathy in men with type 2 diabetes and obstructive sleep apnoea. Diabet Med. 2010. 27:423–30.9.Tahrani AA., Ali A., Raymond NT., Begum S., Dubb K., Altaf QA, et al. Obstructive sleep apnea and diabetic nephropathy: a cohort study. Diabetes Care. 2013. 36:3718–25.10.Tahrani AA., Ali A., Raymond NT., Begum S., Dubb K., Mughal S, et al. Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med. 2012. 186:434–41.11.Seicean S., Strohl KP., Seicean A., Gibby C., Marwick TH. Sleep disordered breathing as a risk of cardiac events in subjects with diabetes mellitus and normal exercise echo-cardiographic findings. Am J Cardiol. 2013. 111:1214–20.
Article12.Poggiogalle E., Jamshed H., Peterson CM. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism. 2018. 84:11–27.
Article13.Pan A., Schernhammer ES., Sun Q., Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011. 8:e1001141.
Article14.Wefers J., van Moorsel D., Hansen J., Connell NJ., Havekes B., Hoeks J, et al. Circadian misalignment induces fatty acid metabolism gene profiles and compromises insulin sensi-tivity in human skeletal muscle. Proc Natl Acad Sci U S A. 2018. 115:7789–94.
Article15.van der Zweerde T., Bisdounis L., Kyle SD., Lancee J., van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. 2019. 48:101208.
Article16.Kothari V., Cardona Z., Chirakalwasan N., Anothaisintawee T., Reutrakul S. Sleep interventions and glucose metabolism: systematic review and meta-analysis. Sleep Med. 2021. 78:24–35.
Article17.Tannas CL. Type 2 diabetes and insomnia: impact on metabolic control. Wayne State University Dissertations. 2012. 624:Available from: https://digitalcommons.wayne.edu/oa_dissertations/624/.18.Nakamura M., Nagamine T. Suvorexant as an orexin antagonist may regulate serum glucose levels in psychiatric patients with insomnia. Psychiatry Clin Neurosci. 2017. 71:844.
Article19.Tan X., van Egmond L., Chapman CD., Cedernaes J., Benedict C. Aiding sleep in type 2 diabetes: therapeutic considerations. Lancet Diabetes Endocrinol. 2018. 6:60–8.
Article