J Cerebrovasc Endovasc Neurosurg.
2024 Dec;26(4):399-404. 10.7461/jcen.2024.E2023.11.007.
Use of a new low-profile coronary stent graft for the treatment of intracranial carotid blow-out
- Affiliations
-
- 1Department of Radiology, Hacettepe University of Medicine of Faculty, Ankara, Turkey
- 2Department of Neurosurgery, Hacettepe University of Medicine of Faculty, Ankara, Turkey
- KMID: 2563089
- DOI: http://doi.org/10.7461/jcen.2024.E2023.11.007
Abstract
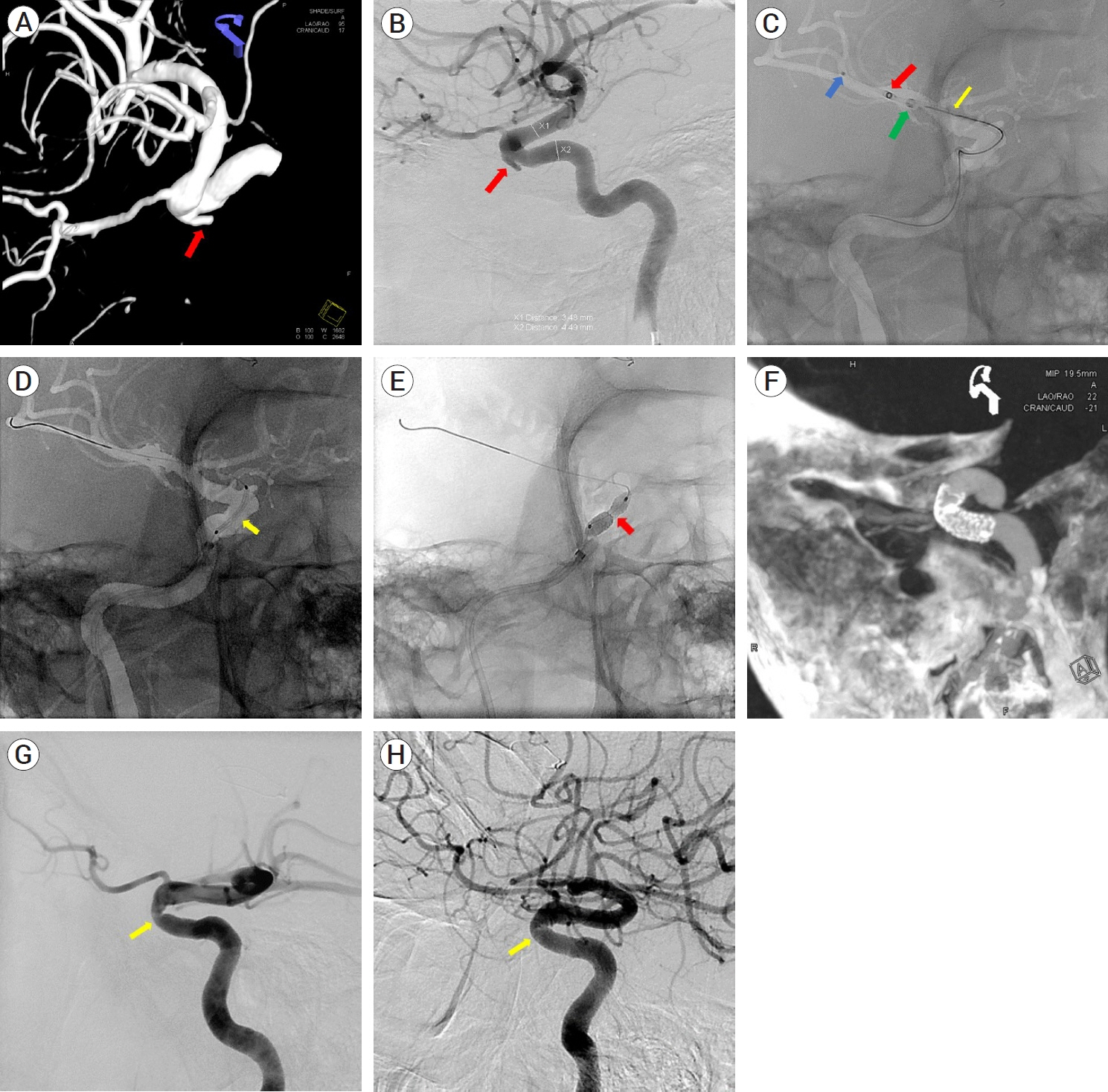
- A 50-year-old male patient with a history of transcranial surgery and subsequent radiotherapy for a pituitary adenoma presented with repetitive pulsatile nasal bleeding. A right cavernous segment pseudoaneurysm was discovered on the angiogram, and the patient failed the balloon occlusion test. A Papyrus (Biotronik, Berlin, Germany) stent graft, which is approved for coronary interventions, was successfully deployed over a coaxial guiding system during the emergent treatment of the false aneurysm. The patient tolerated the procedure well and nasal bleeding did not recur after the procedure. At one-year angiographic follow-up, the stent graft was patent and there was no evidence of recanalization of the false aneurysm.
Keyword
Figure
Reference
-
1. Bond KM, Brinjikji W, Murad MH, Cloft HJ, Lanzino G. Endovascular treatment of carotid blowout syndrome. J Vasc Surg. 2017; 65(3):883–8.
Article2. Chang FC, Luo CB, Lirng GF, Guo WY, Wu HM, Huo Teng MM, et al. Complications of carotid blowout syndrome in patients with head and neck cancers treated by covered stents. Interv Neuroradiol. 2008; 14 Suppl 2(Suppl 2):29–33.
Article3. Chen D, Concus AP, Halbach VV, Cheung SW. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope. 1998; 108(3):326–31.
Article4. Chen SH, McCarthy DJ, Sheinberg D, Hanel R, Sur S, Jabbour P, et al. Pipeline embolization device for the treatment of intracranial pseudoaneurysms. World Neurosurg. 2019; 127:e86–93.
Article5. Deng Q, Feng WF. Efficacy of pipeline endovascular device and Willis stent graft in the treatment of traumatic pseudo intracranial aneurysms. J Interv Med. 2020; 3(1):45–48.
Article6. Gao X, Li Y, Meng L, Tong Z, Guo L, Zhang J, et al. Extra-luminal treatment for an internal carotid artery aneurysm with hostile anatomic condition. Ann Vasc Surg. 2020; 66:669.e17–669.e20.
Article7. Hernández-Enríquez M, Belle L, Madiot H, Pansieri M, Souteyrand G, de Poli F, et al. Use and outcomes of the PK Papyrus covered stent in France: SOS PK Papyrus Registry. Catheter Cardiovasc Interv. 2021; 98(5):874–81.
Article8. Hou K, Wu W, Liu Y, Qu L, Xu B, Yu J. Role of the ophthalmic artery in the endovascular treatment for intracranial vascular diseases. Acta Neurol Belg. 2021; 121(2):321–30.
Article9. Inaraja Pérez GC, Morata AR, Ortega JPR, Medialdea RG, García PK. Endovascular treatment of a symptomatic vertebral artery pseudoaneurysm. Ann Vasc Surg. 2015; 29(5):1018.e5–8.
Article10. Jamshidi N. PK Papyrus coronary stent for the treatment of diminutive and tortuous visceral artery pseudoaneurysms. Cardiovasc Intervent Radiol. 2020; 43(7):1097–8.
Article11. Kalia JS, Niu T, and Zaidat OO. The use of a covered stent graft for obliteration of high-flow carotid cavernous fistula presenting with life-threatening epistaxis. J Neurointerv Surg. 2009; 1(2):142–5.
Article12. Liu C, Shen Y, Qian Y, Hu Y, Hu X, Wu X. Application of covered stent graft in the treatment of complex carotid artery lesions: A single center experience. Vascular. 2022; 30(6):1034–43.
Article13. Liu Y, Yang HF, Xiong ZY, Zheng J, Liu CY, Zhao HY, et al. Efficacy and safety of willis covered stent for treatment of complex vascular diseases of the internal carotid artery. Ann Vasc Surg. 2019; 61:203–11.
Article14. Nagaraja V, Schwarz K, Moss S, Kwok SH, Gunning M. Outcomes of patients who undergo percutaneous coronary intervention with covered stents for coronary perforation: A systematic review and pooled analysis of data. Catheter Cardiovasc Interv. 2020; 96(7):1360–6.
Article15. Topcuoglu OM, Arat A, Peker A, Sarikaya B. Intermediate catheter placement distal to the cerebral aneurysm during flow diversion embolization with the Surpass device. J Neurointerv Surg. 2018; 10(12):e35.
Article16. Touzé R, Touitou V, Shotar E, Gabrieli J, Drir M, Mathon B, et al. Long-term visual outcome in patients treated by flow diversion for carotid-ophthalmic aneurysms. J Neurointerv Surg. 2018; 10(11):1067–73.
Article17. Wong GK, Poon WS. Why current evidence is against flow diverters for treatment of carotid blowout syndrome. Eur J Radiol. 2013; 82(1):191.
Article18. Xu X, Gopinathan A, Ong WK, Thong MKT, Loh WS, Loh KS. Deconstructive versus reconstructive approach to internal carotid artery blowout in radiated nasopharyngeal carcinoma: A tertiary center experience and systematic review. Head Neck. 2023; 45(6):1604–14.
Article19. Zhu YQ, Li MH, Lin F, Song DL, Tan HQ, Gu BX, et al. Frequency and predictors of endoleaks and long-term patency after covered stent placement for the treatment of intracranial aneurysms: A prospective, non-randomised multicentre experience. Eur Radiol. 2013; 23(1):287–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of High-Flow Carotid Cavernous Fistula Using a Graft Stent: Case Report
- Stent-Graft Repair of Common Carotid Pseudoaneurysms in Behcet's Syndrome
- Self-Expandable Stenting over a Stent Graft for the Exclusion of a Carotid Stump: Troubleshooting for Device Incompatibility
- A Case of Transradial Approach to Carotid Artery Angioplasty and Stenting in Left Internal Carotid Stenosis
- Treatment of an Acute Mycotic Aneurysm of the Common Carotid Artery with a Covered Stent-Graft