Ann Hepatobiliary Pancreat Surg.
2024 Nov;28(4):474-482. 10.14701/ahbps.24-117.
Impact of longitudinal tumor location on postoperative outcomes in gallbladder cancer: Fundus and body vs. neck and cystic duct, a retrospective multicenter study
- Affiliations
-
- 1Department of Surgery, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- 2Department of Surgery, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea
- 3Department of Surgery, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University, Daejeon, Korea
- 4Department of Surgery, Naeun Hospital, Incheon, Korea
- 5Department of Surgery, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 6Department of Surgery, Cheongju St. Mary’s Hospital, Cheongju, Korea
- 7Department of Surgery, Daejeon Sun Hospital, Daejeon, Korea
- KMID: 2561580
- DOI: http://doi.org/10.14701/ahbps.24-117
Abstract
- Backgrounds/Aims
Systematic investigations into the prognostic impact of the longitudinal tumor location in gallbladder cancer (GBC) remain insufficient. To address the limitations of our pilot study, we conducted a multicenter investigation to clarify the impact of the longitudinal tumor location on the oncological outcomes of GBC.
Methods
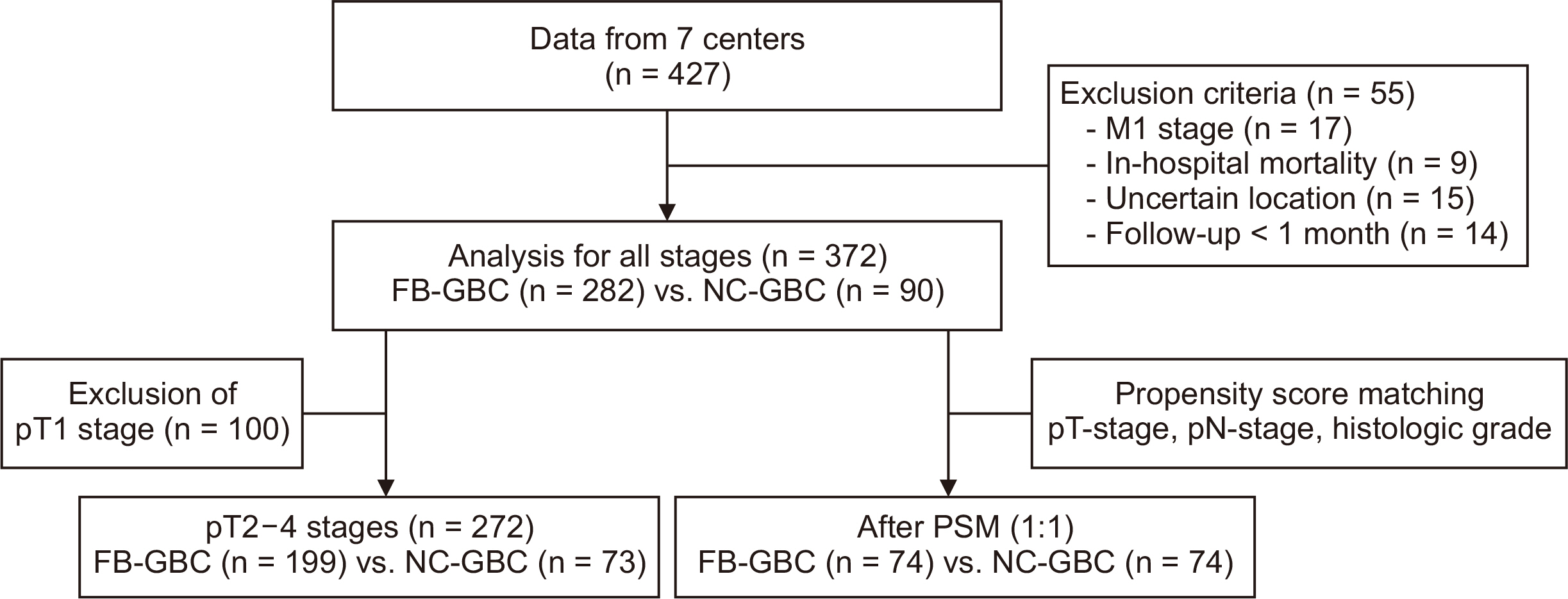
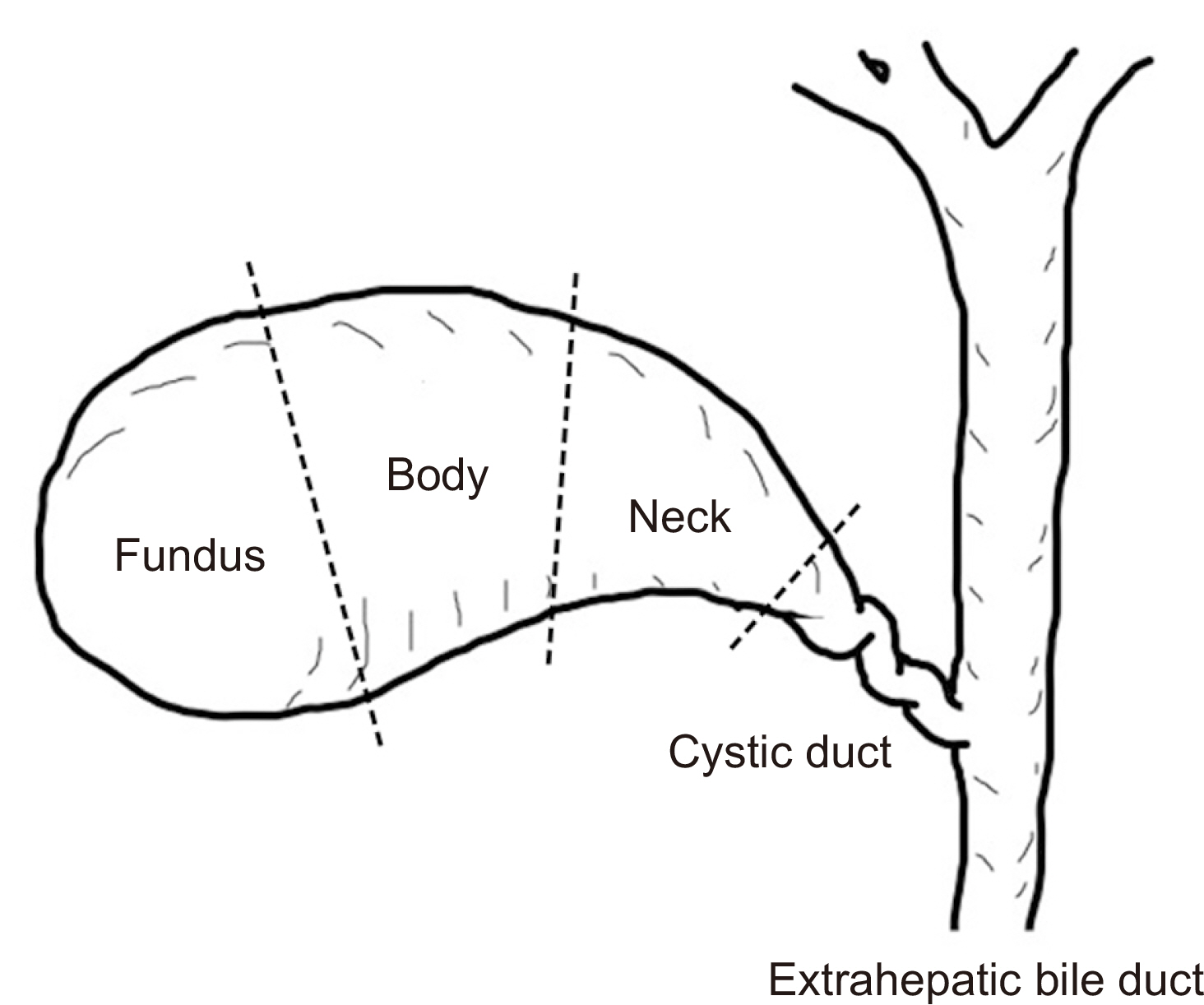
A retrospective multicenter study was conducted on 372 patients undergoing radical resections for GBC from January 2010 to December 2019 across seven hospitals that belong to the Daejeon–Chungcheong branch of the Korean Association of Hepato-Biliary-Pancreatic Surgery. Patients were divided into GBC in the fundus/body (FB-GBC) and GBC in the neck/cystic duct (NC-GBC) groups, based on the longitudinal tumor location.
Results
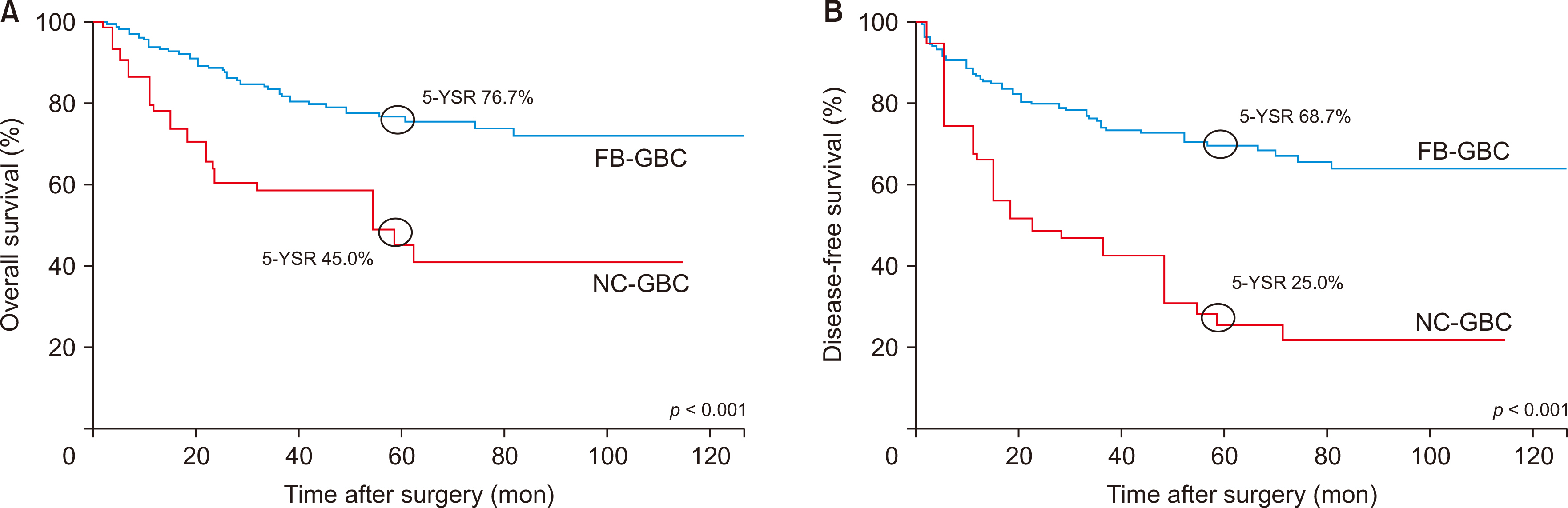
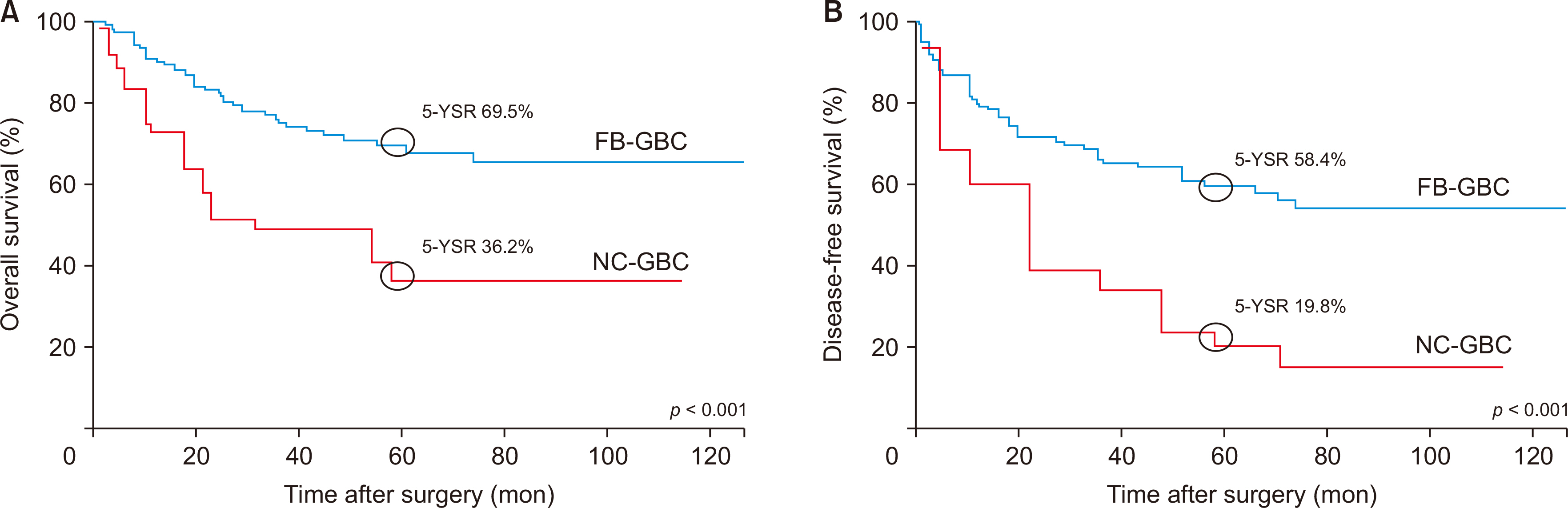
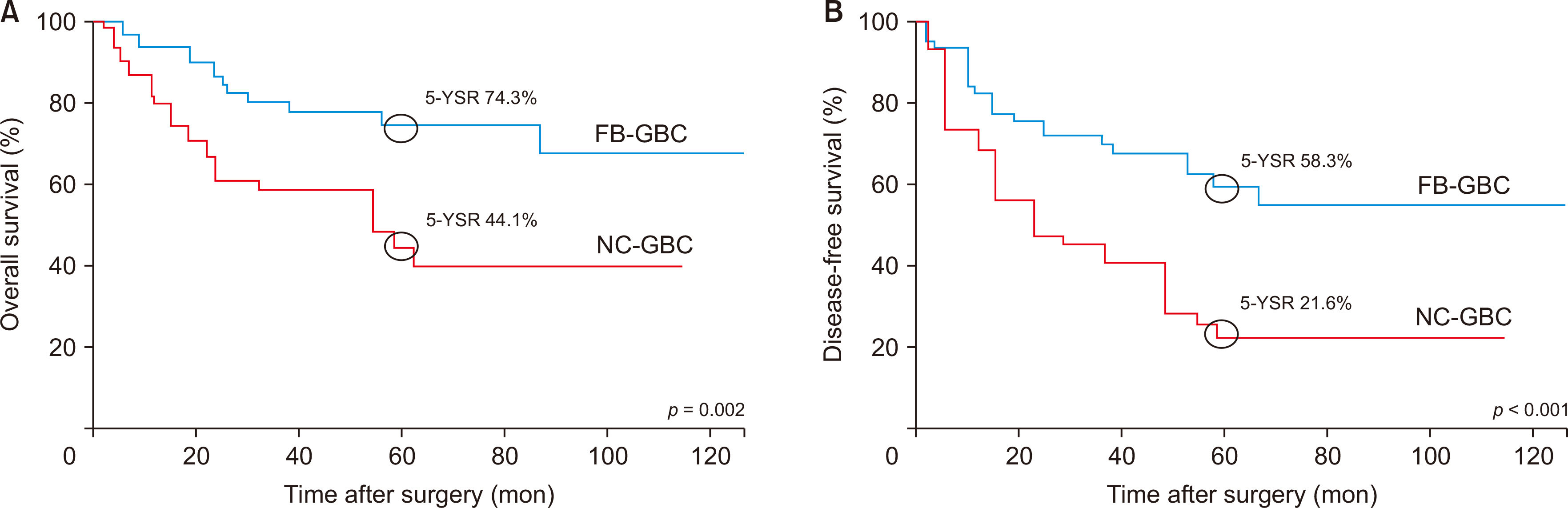
Of 372 patients, 282 had FB-GBC, while 90 had NC-GBC. NC-GBC was associated with more frequent elevation of preoperative carbohydrate antigen (CA) 19-9 levels, requirement for more extensive surgery, more advanced histologic grade and tumor stages, more frequent lymphovascular and perineural invasion, lower R0 resection rates, higher recurrence rates, and worse 5-year overall and disease-free survival rates. Propensity score matching analysis confirmed these findings, showing lower R0 resection rates, higher recurrence rates, and worse survival rates in the NC-GBC group. Multivariate analysis identified elevated preoperative CA 19-9 levels, lymph node metastasis, and non-R0 resection as independent prognostic factors, but not longitudinal tumor location.
Conclusions
NC-GBC exhibits more frequent elevation of preoperative CA 19-9 levels, more advanced histologic grade and tumor stages, lower R0 resection rates, and poorer overall and disease-free survival rates, compared to FB-GBC. However, the longitudinal tumor location was not analyzed as an independent prognostic factor.
Keyword
Figure
Reference
-
References
1. Kang H, Choi YS, Suh SW, Choi G, Do JH, Oh HC, et al. 2021; Prognostic significance of tumor location in T2 gallbladder cancer: a systematic review and meta-analysis. J Clin Med. 10:3317. DOI: 10.3390/jcm10153317. PMID: 34362101. PMCID: PMC8348431.2. Lafaro K, Blakely AM, Melstrom LG, Warner SG, Lee B, Singh G, et al. 2020; Prognostic impact of tumor location in resected gallbladder cancer: a national cohort analysis. J Surg Oncol. 122:1084–1093. DOI: 10.1002/jso.26107. PMID: 32652555. PMCID: PMC8808377.3. Chen C, Geng Z, Shen H, Song H, Zhao Y, Zhang G, et al. 2016; Long-term outcomes and prognostic factors in advanced gallbladder cancer: focus on the advanced T stage. PLoS One. 11:e0166361. DOI: 10.1371/journal.pone.0166361. PMID: 27846279. PMCID: PMC5112857.4. Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC Cancer staging manual. 8th ed. Springer;2017. p. 303–310.5. Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, Zimmitti G, et al. 2015; Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg. 261:733–739. DOI: 10.1097/SLA.0000000000000728. PMID: 24854451. PMCID: PMC4800978.6. Lee W, Jeong CY, Jang JY, Kim YH, Roh YH, Kim KW, et al. 2017; Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer? Results of a retrospective multicenter study. Surgery. 162:515–524. DOI: 10.1016/j.surg.2017.05.004. PMID: 28629653.7. Miyazaki M, Ohtsuka M, Miyakawa S, Nagino M, Yamamoto M, Kokudo N, et al. 2015; Classification of biliary tract cancers established by the Japanese society of hepato-biliary-pancreatic surgery: 3rd english edition. J Hepatobiliary Pancreat Sci. 22:181–196. DOI: 10.1002/jhbp.211. PMID: 25691463.8. Yuan Z, Shui Y, Liu L, Guo Y, Wei Q. 2022; Postoperative recurrent patterns of gallbladder cancer: possible implications for adjuvant therapy. Radiat Oncol. 17:118. DOI: 10.1186/s13014-022-02091-6. PMID: 35799270. PMCID: PMC9264693.9. Lee SE, Jang JY, Lim CS, Kang MJ, Kim SW. 2011; Systematic review on the surgical treatment for T1 gallbladder cancer. World J Gastroenterol. 17:174–180. DOI: 10.3748/wjg.v17.i2.174. PMID: 21245989. PMCID: PMC3020370.10. Aloia TA, Járufe N, Javle M, Maithel SK, Roa JC, Adsay V, et al. 2015; Gallbladder cancer: expert consensus statement. HPB (Oxford). 17:681–690. DOI: 10.1111/hpb.12444. PMID: 26172135. PMCID: PMC4527853.11. Leigh N, Pletcher E, Solomon D, Sarpel U, Labow DM, Magge DR, et al. 2021; The significance of anatomic tumor location in gallbladder cancer. J Surg Oncol. 123:932–938. DOI: 10.1002/jso.26345. PMID: 33368336.12. Nakata T, Kobayashi A, Miwa S, Soeda J, Miyagawa S. 2007; Impact of tumor spread to the cystic duct on the prognosis of patients with gallbladder carcinoma. World J Surg. 31:155–161. discussion 162–163. DOI: 10.1007/s00268-006-0118-1. PMID: 17180477.13. Lv TR, Hu HJ, Liu F, Ma WJ, Jin YW, Li FY. 2023; The significance of peri-neural invasion in patients with gallbladder carcinoma after curative surgery: a 10 year experience in China. Updates Surg. 75:1123–1133. DOI: 10.1007/s13304-023-01519-2. PMID: 37099122.14. Li Y, Song Y, Zhang Y, Liu S. 2022; Progress in gallbladder cancer with lymph node metastasis. Front Oncol. 12:966835. DOI: 10.3389/fonc.2022.966835. PMID: 36072797. PMCID: PMC9441950.15. Wen Z, Si A, Yang J, Yang P, Yang X, Liu H, et al. 2017; Elevation of CA19-9 and CEA is associated with a poor prognosis in patients with resectable gallbladder carcinoma. HPB (Oxford). 19:951–956. DOI: 10.1016/j.hpb.2017.06.011. PMID: 28750922.16. Hatzaras I, Schmidt C, Muscarella P, Melvin WS, Ellison EC, Bloomston M. 2010; Elevated CA 19-9 portends poor prognosis in patients undergoing resection of biliary malignancies. HPB (Oxford). 12:134–138. DOI: 10.1111/j.1477-2574.2009.00149.x. PMID: 20495658. PMCID: PMC2826672.17. D'Angelica M, Dalal KM, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. 2009; Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 16:806–816. DOI: 10.1245/s10434-008-0189-3. PMID: 18985272.18. Kurahara H, Maemura K, Mataki Y, Sakoda M, Iino S, Kawasaki Y, et al. 2018; Indication of extrahepatic bile duct resection for gallbladder cancer. Langenbecks Arch Surg. 403:45–51. DOI: 10.1007/s00423-017-1620-7. PMID: 28875312.19. Kaneoka Y, Yamaguchi A, Isogai M, Harada T, Suzuki M. 2003; Hepatoduodenal ligament invasion by gallbladder carcinoma: histologic patterns and surgical recommendation. World J Surg. 27:260–265. DOI: 10.1007/s00268-002-6702-0. PMID: 12607048.20. Pandey D, Garg PK, Manjunath NM, Sharma J. 2015; Extra-hepatic bile duct resection: an insight in the management of gallbladder cancer. J Gastrointest Cancer. 46:291–296. DOI: 10.1007/s12029-015-9737-9. PMID: 26049726.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic cholecystectomy and common bile duct exploration for gallstone and common bile duct stone in a patient with a left-sided gallbladder: a case report
- Double Primary Cancer of the Gallbladder and Cystic Duct: A Case Report
- Extent of Surgical Resection in Gallbladder Cancer
- Synchronous Double Primary Carcinoma of the Intrahepatic Bile Duct and the Gallbladder
- Double gallbladder completely enclosed in a cystogastric fold of peritoneum