Ewha Med J.
2024 Oct;47(4):e51. 10.12771/emj.2024.e51.
Comparison of the long-term outcomes of cast immobilization methods in distal radius fractures: a systematic review of randomized controlled trials
- Affiliations
-
- 1Orthopaedics and Traumatology Department, Prof. Dr. IGNG Ngoerah General Hospital, Faculty of Medicine Udayana University, Bali, Indonesia
- 2Department of Orthopedic Surgery, St. Carolus Hospital, Jakarta, Indonesia
- 3Faculty of Medicine, Universitas Trisakti, Jakarta, Indonesia
- KMID: 2561416
- DOI: http://doi.org/10.12771/emj.2024.e51
Abstract
Objectives
Conservative treatment for distal radius fractures typically involves closed reduction and immobilization with a plaster cast. However, no consensus exists regarding the best method and duration for immobilization. This study investigated the functional outcomes associated with different plaster cast application techniques in the treatment of stable distal radius fractures.
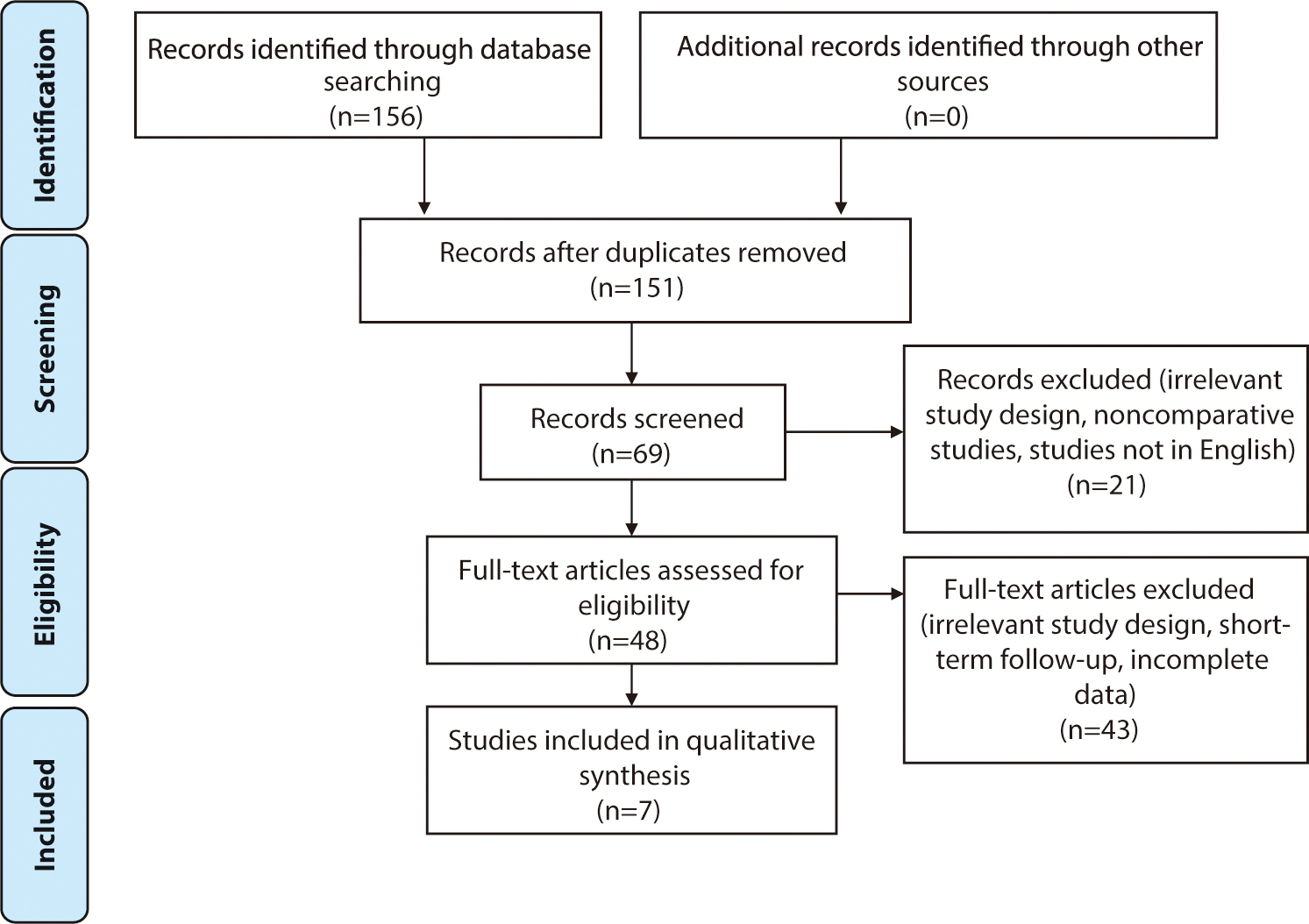
Methods
A systematic search was performed in accordance with PRISMA guidelines for studies in the last 5 years. The inclusion criteria were randomized controlled trials that investigated non-operative treatments for distal radius fractures. We excluded studies with short-term follow-up (less than 3 months), ongoing trials, those that did not directly address fractures, and studies involving the use of sugar-tong splints or non-circular immobilization. The outcomes evaluated included subjective measures (Disabilities of the Arm, Shoulder and Hand score; Patient-Rated Wrist Evaluation score; Mayo Wrist Score; and visual analog scale) and objective outcomes (complication rate and radiological parameters).
Results
We included seven articles from 2017 to 2022. These studies reported a total of 542 fractures, predominantly in women, with a mean age of over 50 years. Both short and long arm casts demonstrated similar functional and radiological outcomes. A longer immobilization period (>3 weeks) should be considered to prevent re-displacement.
Conclusion
In stable fractures treated conservatively, the use of both short and long arm casts resulted in comparable functional outcomes in older patients. Immobilization for at least 3 weeks is recommended, as it provided similar clinical and radiological outcomes compared to longer periods of immobilization (level of evidence: 2A).
Figure
Reference
-
References
1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg. 2001; 26(5):908–915. DOI: 10.1053/jhsu.2001.26322. PMID: 11561245.
Article2. Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg. 2011; 36(5):824–835. DOI: 10.1016/j.jhsa.2011.02.005. PMID: 21527140. PMCID: PMC3093102.3. Gutiérrez-Monclus R, Gutiérrez-Espinoza H, Zavala-González J, Olguín-Huerta C, Rubio-Oyarzún D, Araya-Quintanilla F. Correlation between radiological parameters and functional outcomes in patients older than 60 years of age with distal radius fracture. Hand. 2019; 14(6):770–775. DOI: 10.1177/1558944718770203. PMID: 29661068. PMCID: PMC6900695.
Article4. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annu Intern Med. 2009; 151(4):264–269. DOI: 10.7326/0003-4819-151-4-200908180-00135. PMID: 19622511.
Article5. Furlan AD, Malmivaara A, Chou R, Maher C, Deyo RA, Schoene M, et al. Updated method guideline for systematic reviews in the cochrane back and neck group. Spine. 2015; 40(21):1660–1673. DOI: 10.1097/BRS.0000000000001061. PMID: 26208232.
Article6. Park MJ, Kim JP, Lee HI, Lim TK, Jung HS, Lee JS. Is a short arm cast appropriate for stable distal radius fractures in patients older than 55 years? A randomized prospective multicentre study. J Hand Surg Eur Vol. 2017; 42(5):487–492. DOI: 10.1177/1753193417690464. PMID: 28490225.
Article7. Caruso G, Tonon F, Gildone A, Andreotti M, Altavilla R, Valentini A, et al. Below-elbow or above-elbow cast for conservative treatment of extra-articular distal radius fractures with dorsal displacement: a prospective randomized trial. J Orthop Surg Res. 2019; 14:477. DOI: 10.1186/s13018-019-1530-1. PMID: 31888682. PMCID: PMC6937655.8. Okamura A, de Moraes VY, Neto JR, et al. No benefit for elbow blocking on conservative treatment of distal radius fractures: A 6-month randomized controlled trial. PLoS One. 2021; 16(6):0252667. DOI: 10.1371/journal.pone.0252667. PMID: 34111160. PMCID: PMC8191961.9. Christersson A, Larsson S, Sandén B. Clinical outcome after plaster cast fixation for 10 days versus 1 month in reduced distal radius fractures: a prospective randomized study. Scand J Surg. 2018; 107(1):82–90. DOI: 10.1177/1457496917731184. PMID: 28942705.
Article10. Bentohami A, van Delft EAK, Vermeulen J, Sosef NL, de Korte N, Bijlsma TS, et al. Non- or minimally displaced distal radial fractures in adult patients: three weeks versus five weeks of cast immobilization: a randomized controlled trial. J Wrist Surg. 2019; 8(01):043–048. DOI: 10.1055/s-0038-1668155. PMID: 30723601. PMCID: PMC6358449.11. Boersma EZ, Hekma EJ, Kraaijvanger N, Mollen RMHG, Nijhuis-van der Sanden MWG, Edwards MJR. Cast-OFF Trial: one versus 4 to 5 weeks of plaster cast immobilization for nonreduced distal radius fractures: a randomized clinical feasibility trial. Hand. 2022; 17:1_suppl. 60S–69S. DOI: 10.1177/15589447211044775. PMID: 34569335. PMCID: PMC9793615.12. Olech J, Kopczyński B, Tomczyk , Konieczny G, Kazubski K, Morasiewicz P. The functional and radiographic outcomes following distal radius fracture treatment in a cast for 4 and 6 weeks in the elderly: a randomized trial. Adv Clin Exp Med. 2022; 31(6):701–706. DOI: 10.17219/acem/150032. PMID: 35652298.
Article13. Diaz-Garcia RJ, Chung KC. The evolution of distal radius fracture management: a historical treatise. Hand Clin. 2012; 28(2):105–111. DOI: 10.1016/j.hcl.2012.02.007. PMID: 22554653. PMCID: PMC3345122.
Article14. Saving J, Severin Wahlgren S, Olsson K, Enocson A, Ponzer S, Sköldenberg O, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg. 2019; 101(11):961–969. DOI: 10.2106/JBJS.18.00768. PMID: 31169572.
Article15. Bong MR, Egol KA, Leibman M, Koval KJ. A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg. 2006; 31(5):766–770. DOI: 10.1016/j.jhsa.2006.01.016. PMID: 16713840.
Article16. Hohmann E, Meta M, Navalgund V, Tetsworth K. The relationship between radiological alignment of united distal radius fractures and functional and patient-perceived outcomes in elderly patients. J Orthop Surg. 2017; 25(1):2309499016684976. DOI: 10.1177/2309499016684976. PMID: 28193139.17. Kwok IHY, Leung F, Yuen G. Assessing results after distal radius fracture treatment: a comparison of objective and subjective tools. Geriatr Orthop Surg Rehabil. 2011; 2(4):155–160. DOI: 10.1177/2151458511422701. PMID: 23569685. PMCID: PMC3597314.
Article18. Dacombe PJ, Amirfeyz R, Davis T. Patient-reported outcome measures for hand and wrist trauma: is there sufficient evidence of reliability, validity, and responsiveness? Hand. 2016; 11(1):11–21. DOI: 10.1177/1558944715614855. PMID: 27418884. PMCID: PMC4920509.19. Kleinlugtenbelt YV, Nienhuis RW, Bhandari M, Goslings JC, Poolman RW, Scholtes VAB. Are validated outcome measures used in distal radial fractures truly valid? Bone Joint Res. 2016; 5(4):153–161. DOI: 10.1302/2046-3758.54.2000462. PMID: 27132246. PMCID: PMC4921040.
Article20. Webb GR, Galpin RD, Armstrong DG. Comparison of short and long arm plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg. 2006; 88(1):9–17. DOI: 10.2106/JBJS.E.00131. PMID: 16391244.
Article21. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989; 20(4):208–210. DOI: 10.1016/0020-1383(89)90113-7. PMID: 2592094.
Article22. Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles’ fractures. Functional bracing in supination. J Bone Joint Surg. 1975; 57(3):311–317. DOI: 10.2106/00004623-197557030-00004.23. Raittio L, Launonen AP, Hevonkorpi T, Luokkala T, Kukkonen J, Reito A, et al. Two casting methods compared in patients with Colles’ fracture: a pragmatic, randomized controlled trial. PLoS One. 2020; 15(5):0232153. DOI: 10.1371/journal.pone.0232153. PMID: 32469881. PMCID: PMC7259650.24. van Delft EAK, van Gelder TG, de Vries R, Vermeulen J, Bloemers FW. Duration of cast immobilization in distal radial fractures: a systematic review. J Wrist Surg. 2019; 08(05):430–438. DOI: 10.1055/s-0039-1683433. PMID: 31579555. PMCID: PMC6773589.25. de Bruijn MAN, van Ginkel LA, Boersma EZ, van Silfhout L, Tromp TN, van de Krol E, et al. Cast immobilization duration for distal radius fractures, a systematic review. Eur J Trauma Emerg Surg. 2024; Mar. 20. [Epub]. DOI: 10.1007/s00068-024-02494-y. PMID: 38507086. PMCID: PMC11458645.26. Saka N, Hoshika S, Inoue M, Watanabe J, Banno M. Below- or above-elbow immobilization in conservative treatment of distal radius fractures: a systematic review and meta-analysis. Injury. 2022; 53(2):250–258. DOI: 10.1016/j.injury.2021.12.021. PMID: 34961625.
Article27. Raj V, Barik S, Richa . Comparison of above elbow and below elbow immobilisation for conservative treatment of distal end radius fracture in adults: a systematic review and meta-analysis of randomized clinical trials. Chin J Traumatol. 2023; 26(4):204–210. DOI: 10.1016/j.cjtee.2022.12.005. PMID: 36737394. PMCID: PMC10388250.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors in Stability after Immobilization of the Distal Radius in Unstable Fractures in Children
- Treatment of Ulnar Fractures Combined with Distal Radius Fracture
- Treatment of Comminuted Distal Radius Fracutures with External Skeletal Fixation
- Closed Reduction and Cast Immobilization for the Treatment of Distal Radius Fracture: Does Dorsal Metaphyseal Comminution Predict Radiographic and Functional Outcomes?
- Complications of Distal Radius Fracture